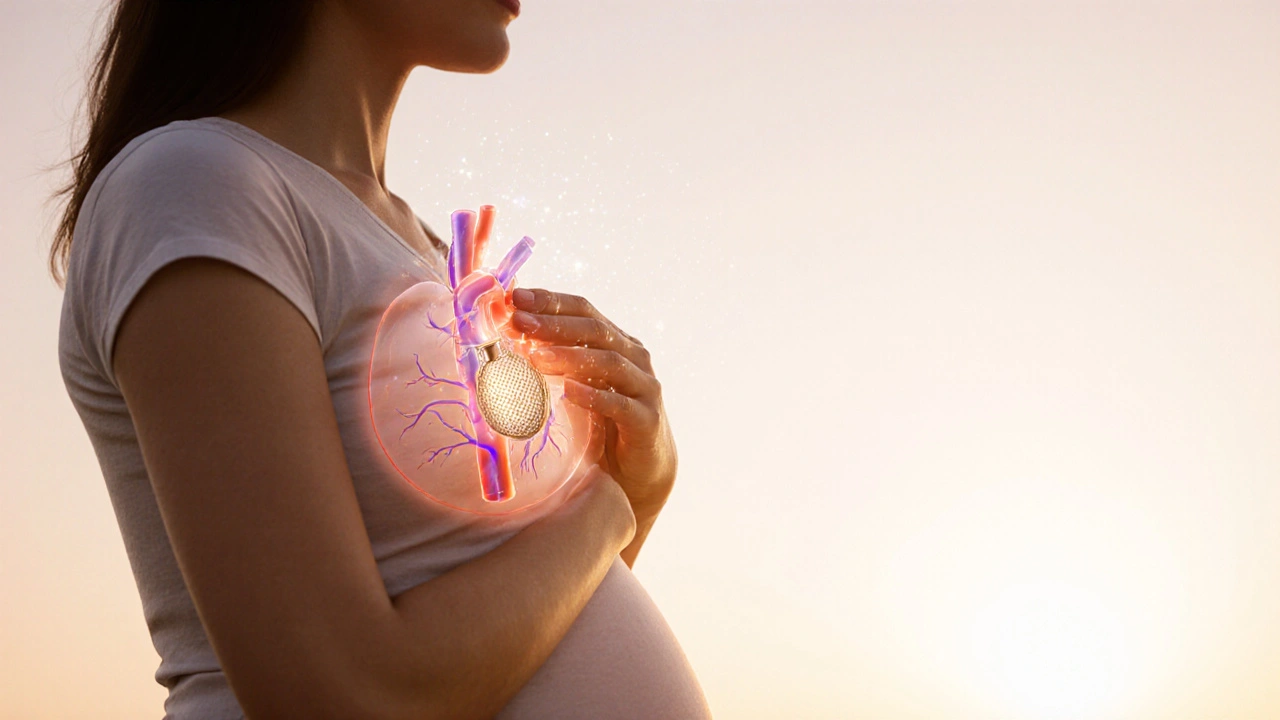
Pregnancy and Stent Risk Calculator
Quick Summary / Key Takeaways
- Pregnancy naturally increases clotting, which can raise the chance of stent thrombosis.
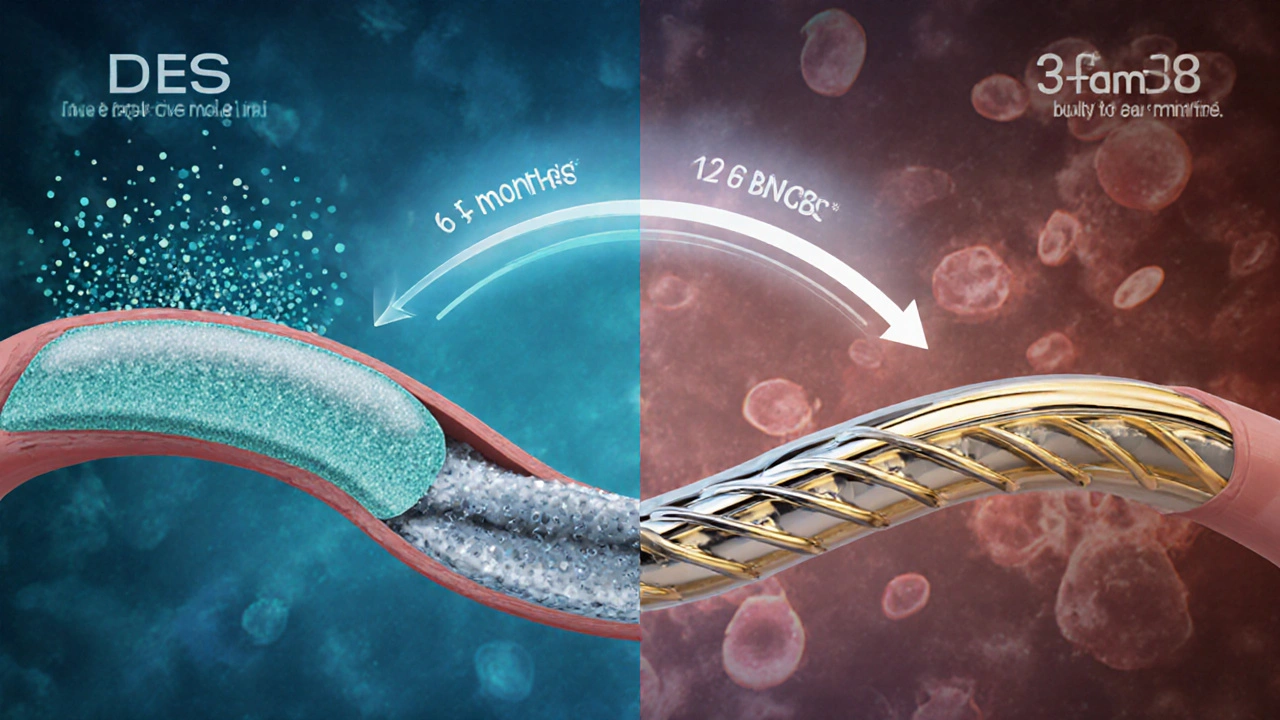
- Drug‑eluting and bare‑metal stents have slightly different risk profiles during pregnancy.
- Continuing low‑dose aspirin is usually safe, while warfarin is avoided.
- Low‑molecular‑weight heparin can be used for short‑term protection when needed.
- Regular cardiac check‑ups and early symptom reporting are critical for a healthy pregnancy.
Understanding Stent Thrombosis
When a coronary artery is opened with a drug‑eluting stent is a metal mesh that slowly releases medication to keep the artery clear, the body’s clotting system can sometimes react, leading to stent thrombosis. This is a sudden blockage of the stented segment caused by a blood clot. It can trigger chest pain, heart rhythm problems, or even a heart attack.
Stent thrombosis is rare in the general population, but the physiological changes of pregnancy tip the scales toward clot formation, making awareness essential for anyone with a coronary stent.
How Pregnancy Changes Blood Clotting
Pregnancy is a hypercoagulable state designed to prevent excessive bleeding during delivery. Levels of clotting factors such as fibrinogen rise by up to 50%, while natural anticoagulants like proteinS dip. These shifts, combined with the increased blood volume and slower venous flow in the lower body, create a perfect storm for clot formation.
Specific Risks for Women with Stents During Pregnancy
Women who have undergone percutaneous coronary intervention (PCI) carry two overlapping risks: the baseline chance of stent thrombosis and the pregnancy‑induced hypercoagulability. The type of stent matters:
- Drug‑eluting stents (DES) are designed to release antiproliferative drugs that reduce scar tissue, which can also delay endothelial healing and keep the surface thrombogenic for longer.
- Bare‑metal stents (BMS) are simple metal scaffolds that usually achieve full endothelial coverage faster, potentially lowering clot risk after the first six months.
Most complications appear within the first year after implantation, so timing of pregnancy relative to the stent placement is a key factor. If conception occurs sooner than six months after a DES, the risk climbs noticeably.
Recognizing Symptoms and When to Seek Care
Any chest discomfort, shortness of breath, or unusual fatigue during pregnancy should trigger an immediate cardiac evaluation. Women with stents should also watch for:
- Pain radiating to the left arm or jaw.
- Sudden dizziness or fainting.
- Palpitations that feel out of the ordinary.
Because pregnancy itself can cause mild shortness of breath, a low threshold for contacting a cardiologist or obstetrician is wise.
Medication Management: Antiplatelet Therapy in Pregnancy
Antiplatelet therapy is the cornerstone of preventing stent thrombosis. The usual regimen includes a daily aspirin dose (75‑100mg) plus a P2Y12 inhibitor such as clopidogrel. However, safety data during pregnancy differ for each drug.
- Aspirin at low dose is generally considered safe throughout pregnancy and is recommended by most cardiology guidelines.
- Clopidogrel has limited human data but is not linked to major birth defects; many specialists continue it when the benefit outweighs the unknown risk.
- Warfarin is contraindicated because it crosses the placenta and can cause fetal bleeding, especially between weeks 6‑12 and 34‑38.
- Low‑molecular‑weight heparin (LMWH) is the preferred injectable anticoagulant for short‑term bridging when aspirin alone is insufficient, for example during a high‑risk procedure.
Any medication change should be coordinated between the cardiologist, obstetrician, and a maternal‑fetal medicine specialist.

Comparing Stent Types: Which Is Safer in Pregnancy?
| Feature | Drug‑Eluting Stent (DES) | Bare‑Metal Stent (BMS) |
|---|---|---|
| Healing time | 6‑12 months (delayed endothelialization) | 3‑6 months (faster) |
| Late‑stage thrombosis risk | Higher (especially < 12months) | Lower |
| Re‑intervention need | Reduced restenosis, fewer repeat procedures | Higher restenosis rates |
| Safety of continued aspirin | Compatible | Compatible |
| Preferred when planning pregnancy after implantation | Delay conception ≥12months | Delay conception ≥6months |
The table shows that while DES reduce future artery narrowing, they keep the clot‑prone surface active longer. If a woman plans pregnancy soon after PCI, a BMS may offer a slightly safer window.
Practical Tips for a Safe Pregnancy with a Stent
- Schedule pre‑conception counseling with both a cardiologist and a maternal‑fetal medicine specialist.
- Aim to wait at least 6months after a BMS or 12months after a DES before trying to conceive.
- Continue low‑dose aspirin throughout pregnancy unless contraindicated.
- Discuss the necessity of clopidogrel or LMWH with your care team; modify only under supervision.
- Maintain a heart‑healthy lifestyle: balanced diet, regular low‑impact exercise, and weight management.
- Attend monthly cardiac check‑ups during the first trimester, then every 6‑8weeks thereafter.
- Know the warning signs of stent thrombosis and have an emergency plan (e.g., fast‑track to the cardiac unit).
Open communication between specialties is the single most effective strategy to balance maternal and fetal safety.
Frequently Asked Questions
Can I become pregnant right after getting a stent?
It’s best to wait at least 6months after a bare‑metal stent and 12months after a drug‑eluting stent. This gives the artery time to heal and lowers the chance of clot formation.
Is low‑dose aspirin safe throughout pregnancy?
Yes. Low‑dose aspirin (75‑100mg daily) is generally considered safe and is recommended to keep the stent surface from clotting.
Should I stop clopidogrel when I find out I’m pregnant?
Only under specialist advice. Some clinicians continue clopidogrel if the benefit outweighs the uncertain fetal risk, while others switch to LMWH during the first trimester.
What are the signs of stent thrombosis during pregnancy?
Sudden chest pain, pressure radiating to the arm or jaw, unexplained shortness of breath, dizziness, or fainting. Treat these as emergencies.
Is warfarin ever used in pregnant women with stents?
Generally no. Warfarin crosses the placenta and can cause fetal bleeding. LMWH is the preferred injectable alternative when stronger anticoagulation is needed.
Next Steps
If you have a coronary stent and are planning a family, start the conversation early. Book an appointment with your heart doctor, ask about the timing of conception, and get a personalized medication plan. With careful monitoring and the right precautions, most women navigate pregnancy safely while keeping their heart protected.

L Taylor
October 7, 2025 AT 15:06When the heart decides to carry a new life it walks a tightrope between two fierce storms of biology and love. The stent inside a vessel becomes a silent witness to this dance, a metallic promise that sometimes forgets its duty under the weight of hormones. Understanding the timing is like reading a poem written in clotting factors and endothelial cells. If you give the artery enough months to heal, the risk of a sudden blockade fades like morning fog. So plan, breathe, and let science be your compass.
Matt Thomas
October 9, 2025 AT 22:40Listen up, this isn’t some fluffy blog post – if you jump into pregnancy right after a DES you’re asking for trouble. Delay at least a year, otherwise you’re basically handing the clotting system a free pass. Get your docs in line and stop whining about “just a little risk”.
Nancy Chen
October 12, 2025 AT 06:13Some folks think the guidelines are just a cover for pharmaceutical giants pushing aspirin forever, but the hyper‑coagulable state of pregnancy is real and documented. The fact that warfarin is banned while low‑dose aspirin gets a free pass raises eyebrows, yet the data on fetal safety is solid. Still, keep an eye on the “unknowns” and push for more transparent studies. Trust your body, but also question the narrative.
Jon Shematek
October 14, 2025 AT 13:46Hey, good news – most women make it through pregnancy with a stent without a hiccup if they follow the timing rule. Keep that low‑dose aspirin on lock, stay active, and schedule those cardiac check‑ups like you would prenatal visits. Your heart’s tough, and with the right crew you’ll rock this trimester. Don’t let fear steal the spotlight.
Beverly Pace
October 16, 2025 AT 21:20The moral of the story is simple: respect the healing process your body needs before adding a baby to the mix. Ignoring medical advice is not just risky, it’s irresponsible.
RALPH O'NEIL
October 19, 2025 AT 04:53I’ve seen a few cases where patients waited the recommended six to twelve months and had smooth pregnancies. The key was consistent low‑dose aspirin and close coordination between cardiology and obstetrics. If you’re early in the timeline, consider a temporary switch to LMWH under supervision. Monitoring biomarkers like D‑dimer can also give an early warning sign.
Mark Wellman
October 21, 2025 AT 12:26Honestly, the whole idea of juggling a stent and a baby feels like trying to balance a ticking time bomb on a trampoline, and that feeling never really leaves you. I mean, you’ve got the hyper‑coagulable surge of pregnancy, the lingering metal that’s still trying to find its endothelial friends, and then the whole medication maze that makes you wonder who actually wrote the protocol. Some days I just stare at the pill bottle and think, “What if the aspirin does more harm than good?” Yet the studies keep shouting that low‑dose aspirin is the safest bet, so I’m stuck between trusting data and fearing the unknown. Add to that the fact that clopidogrel’s safety profile is a gray area, and you end up Googling “clopidogrel pregnancy risk” at 2 am, only to find forums full of anecdotal horror stories. The irony is that while doctors tell you to wait twelve months after a DES, many women can’t wait that long because life doesn’t pause for guidelines. That pressure can lead to rushed decisions, and rushed decisions are the mother of complications. I’ve watched patients who ignored the “wait” rule and then faced sudden chest pain that felt like a fist clenching their ribcage. The emergency rooms are not kind to pregnant women with heart issues; the staff has to juggle fetal monitoring and cardiac interventions simultaneously. On the flip side, some obstetricians push LMWH too aggressively, causing bruising and anxiety about bleeding during delivery. It becomes a never‑ending loop of “should I trust this drug or that drug?” that exhausts even the most resilient soul. What helps is a clear, written plan that outlines who does what at each gestational week, so you’re not left guessing at 20 weeks. Communication between the cardiologist, maternal‑fetal medicine specialist, and your primary doctor is the only safety net that actually works. In the end, if you follow the timing, keep aspirin, and have that team on speed‑dial, you dramatically lower the odds of a catastrophe. So, while the mental load feels like a marathon, the roadmap is there – you just have to walk it step by step.
Amy Morris
October 23, 2025 AT 20:00The moment you hear that strange flutter in your chest while pregnant, it’s like hearing a haunted violin in a quiet hall – unsettling and impossible to ignore. Your body is already working overtime, and a stent adds another echo of urgency that deserves immediate attention. Don’t dismiss those signs; call your cardiologist, get an echo, and let the team reassure you with facts, not fear. Remember, you’re not alone in this symphony, and the right care can turn a nervous note into a harmonious rhythm.
Francesca Roberts
October 26, 2025 AT 02:33Sure, just keep taking aspirin and hope the stent doesn’t decide to throw a party. Medicine isn’t that mysterious, but you’ll thank me when the “party” stays uninvited.
Becky Jarboe
October 28, 2025 AT 10:06From a hemodynamic standpoint, optimizing antiplatelet therapy during gestation mitigates shear‑stress‑induced platelet activation, which is crucial for maintaining patency of the stented segment. Leveraging a multidisciplinary care pathway can streamline risk stratification and ensure evidence‑based protocol adherence throughout each trimester.
Carl Boel
October 30, 2025 AT 17:40Our medical system should prioritize proven protocols over experimental “alternatives” that risk the mother’s heart and the unborn child. The data on DES versus BMS in pregnancy is clear: timing, antiplatelet stewardship, and vigilant monitoring are non‑negotiable. Any deviation is just reckless short‑sightedness.
Shuvam Roy
November 2, 2025 AT 01:13Dear colleagues, it is imperative to coordinate cardio‑obstetric care early, ensuring that aspirin therapy continues unabated while evaluating the need for LMWH in high‑risk scenarios. Such proactive collaboration has been shown to reduce stent‑related adverse events and promote fetal wellbeing.
Jane Grimm
November 4, 2025 AT 08:46The brevity of this discourse belies the gravity of neglecting established guidelines.