Switching from a brand-name antiseizure medication to a generic version might seem like a simple cost-saving move-until it isn’t. For people with epilepsy, even small changes in how a drug is absorbed can mean the difference between staying seizure-free and facing a dangerous breakthrough seizure. This isn’t theoretical. It’s happening in pharmacies across the UK and the US, often without patients or even their doctors fully understanding the risks.
Why Generic Substitution Can Be Risky for Antiseizure Drugs
Many antiseizure medications (ASMs) have a narrow therapeutic index. That means the gap between a dose that works and a dose that causes harm is tiny. For drugs like lamotrigine, carbamazepine, and valproic acid, a 15-20% change in blood levels can trigger seizures or serious side effects like dizziness, confusion, or liver damage. The FDA says generics are bioequivalent if their blood concentration falls within 80-125% of the brand-name drug. That sounds precise-but in practice, it’s a wide range. Two different generics of the same drug could vary by 45% in absorption. For someone on a stable dose of lamotrigine, that could mean their body suddenly gets too little or too much of the drug. And because seizures don’t announce themselves with warning signs, the first sign of trouble might be a fall, a hospital visit, or worse. A 2008 study in Neurology found that patients switched to generic lamotrigine had 23% more doctor visits and 18% more hospitalizations than those who stayed on the brand. A global survey of 1,247 healthcare professionals in 2022 showed 40% of clinicians had seen increased seizure frequency after a generic switch. These aren’t outliers. They’re patterns.Real Stories Behind the Numbers
Patient experiences tell a different story than regulatory reports. On epilepsy forums, the same themes keep appearing:- "I switched from Lamictal to generic lamotrigine and had three seizures in two weeks-something I hadn’t had in five years."
- "The pill changed color and shape every time I refilled. I started doubting if I was taking the right one. My anxiety spiked-and so did my seizures."
- "My 78-year-old mom with dementia couldn’t tell the difference between pills. She took the wrong dose twice. We ended up in A&E."
Regulators Don’t Agree
The FDA maintains that generics are safe and that seizure breakthroughs happen regardless of formulation. But other agencies see it differently. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) explicitly warns that consistency of supply matters for drugs where therapeutic failure could be life-threatening. The European Medicines Agency uses tighter bioequivalence standards for narrow therapeutic index drugs than the FDA does. Even within the medical community, there’s division. Dr. Jacqueline French, a leading neurologist and Chief Medical Officer of the Epilepsy Foundation, supports FDA standards-but adds a critical caveat: "Heightened caution is needed for medically complex patients." Meanwhile, Dr. Philip Glass at Montefiore Medical Center says the evidence is clear: "Even small variations matter." And it’s not just doctors. A 2018 study in Epilepsia found that 27% of patients who switched to a generic ASM switched back to the brand within a year-more than double the rate seen with other types of medications.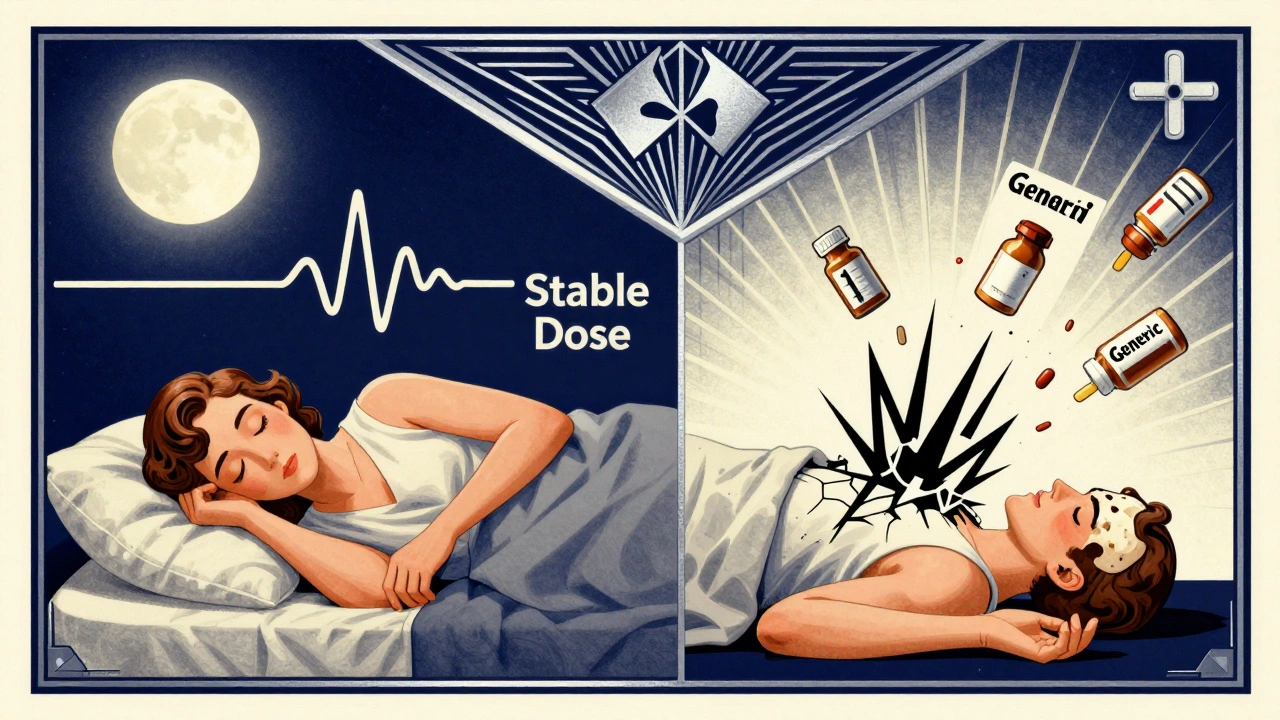
What Makes Some ASMs More Dangerous to Switch?
Not all antiseizure drugs carry the same risk. The ones that cause the most problems share a few traits:- Narrow therapeutic index - small changes in blood levels cause big effects
- Extended-release formulations - generics may release the drug differently, even if the total amount is the same
- Complex metabolism - drugs like carbamazepine interact with other medications, and small changes can throw off the whole balance
- High seizure risk - patients with frequent seizures, drug-resistant epilepsy, or a history of status epilepticus are most vulnerable
Best Practices: How to Stay Safe
If you’re on an antiseizure medication, here’s what you can do:- Ask your neurologist before any switch. Not your pharmacist. Not your GP. Your epilepsy specialist. They know your history, your seizure pattern, and your medication’s behavior in your body.
- Request a consistent brand or generic. If you’ve been stable on a particular version, ask your doctor to write "Dispense as written" or "Do not substitute" on the prescription. Pharmacists are legally required to follow that.
- Know your pills. Take a photo of your medication when you first get it. Note the color, shape, and imprint. If it changes unexpectedly, call your pharmacy and your doctor.
- Track your symptoms. Keep a simple log: date, seizure count, side effects, mood changes. If you notice a pattern after a switch, bring it to your neurologist immediately.
- Check for hidden ingredients. Some generics use fillers with carbohydrates or lactose. For people on the ketogenic diet, even small amounts can disrupt ketosis and trigger seizures.
What’s Being Done About It?
The American Epilepsy Society is running a multi-center study (NCT04987654) tracking seizure outcomes in patients who switch versus those who stay on the same formulation. Early data suggests that even patients who seem stable may have subtle changes in brain activity after a switch. The FDA is also considering tighter standards for narrow therapeutic index drugs-proposing a range of 90-111% instead of 80-125%. But pharmaceutical companies are pushing back, arguing it would reduce access to affordable generics. Meanwhile, the 2024 International Epilepsy Guidelines now recommend an individualized approach to substitution. No more blanket rules. Each patient’s risk must be assessed based on seizure type, frequency, age, cognitive function, and comorbidities.The Bottom Line
Generic antiseizure medications save money-sometimes hundreds of pounds a year. But for people with epilepsy, cost savings shouldn’t come at the cost of safety. The science and the stories both point to one thing: consistency matters. If you’re on an ASM, don’t assume a generic is the same. Ask questions. Know your options. Advocate for yourself. Your brain deserves more than a pill that looks similar-it deserves a dose you can trust.Can I switch from brand-name to generic antiseizure medication safely?
It depends. For some people, switching is fine. For others-especially those with frequent seizures, drug-resistant epilepsy, or cognitive issues-it can be dangerous. Always talk to your neurologist first. Never let a pharmacist switch your medication without your doctor’s approval.
Why do some generics cause more seizures than others?
Even though generics meet FDA bioequivalence standards, they can differ in how quickly they’re absorbed, how they’re released over time, or what fillers they contain. Extended-release versions are especially tricky-small differences in the coating or granule size can change how the drug enters your bloodstream. That’s enough to throw off seizure control in sensitive individuals.
What should I do if I notice more seizures after a generic switch?
Contact your neurologist right away. Keep a seizure diary with dates, times, and possible triggers. Bring your medication bottle to your appointment. Your doctor may need to switch you back to your original formulation or adjust your dose. Don’t wait-early intervention can prevent serious complications.
Can my pharmacist switch my antiseizure medication without telling me?
In the UK and US, pharmacists can substitute generics unless the prescription says "Dispense as written" or "Do not substitute." Always check your prescription label. If you’re unsure, ask your pharmacist if a change was made-and confirm with your doctor if you’re concerned.
Are there any antiseizure medications that are safer to switch?
Some older ASMs like phenytoin and sodium valproate have more predictable absorption and are less likely to cause problems with substitution. But even these aren’t risk-free. Newer drugs like cenobamate and fenfluramine have complex pharmacokinetics and should never be switched without specialist oversight.
Is there financial help if I can’t afford the brand-name drug?
Yes. The Epilepsy Foundation’s Medication Access Program helps over 12,000 patients annually with co-pays and free medication. Your neurologist can help you apply. In the UK, the NHS may cover brand-name drugs if there’s a clinical need. Always ask-don’t assume you can’t afford to stay on what works.


Declan Flynn Fitness
December 3, 2025 AT 05:36Been on lamotrigine for 8 years. Switched to generic once-three days in, I had a night seizure. Never again. My neuro told me to stick with the brand or get a "dispense as written" note. Worth every penny.
Also, take a pic of your pill when you get it. Color, shape, imprint. If it changes, call your pharmacy. It’s not paranoia-it’s survival.
Patrick Smyth
December 4, 2025 AT 19:44I can't believe we're still having this conversation. My sister had a status epilepticus after they switched her to generic carbamazepine. She was fine for years. Then-poof. A pharmacy technician decided what was safe for her. No consent. No warning. Just a cheaper pill. This isn't healthcare. It's corporate roulette.
Irving Steinberg
December 5, 2025 AT 08:24Y’all are overreacting 😅 I switched to generic Keppra and nothing happened. People just need to chill. Also why is everyone so obsessed with pills looking different? It’s not a tattoo. It’s medicine. 🤷♂️
Kshitij Shah
December 6, 2025 AT 11:37In India, we don’t even have brand-name ASMs in rural areas. We get generics that cost 1/10th. Some work. Some don’t. We don’t get to choose. The real issue? No neurologist within 200 km. So yes, the science is valid-but so is the reality that for most of the world, "safe substitution" is a luxury.
Michelle Smyth
December 7, 2025 AT 05:43Let’s be clear: the FDA’s 80–125% bioequivalence window is a statistical fiction masquerading as clinical safety. It’s the kind of regulatory sleight-of-hand that would make a derivatives trader blush. The narrow therapeutic index of ASMs demands precision-not probabilistic approximations. We’re not talking about ibuprofen here. We’re talking about the electrical architecture of the human cortex. To treat it like a commodity is not just negligent-it’s ontologically arrogant.
And yet, the pharmaceutical-industrial complex thrives on this epistemic violence. The same corporations that profit from the brand-name drug then produce the generic under a different label, with different fillers, different dissolution profiles, and the same profit margin. The patient becomes the sacrificial variable in a cost-benefit equation written in blood.
Meanwhile, the WHO lists valproate as essential-but ignores that in low-resource settings, the generics often contain 60% of the labeled dose. This isn’t access. It’s pharmacological colonialism.
And don’t get me started on the "dispense as written" clause. It’s a Band-Aid on a hemorrhage. The system is designed to optimize for throughput, not for neurological integrity. We’ve outsourced the sanctity of the brain to supply chain logistics.
It’s not about fear. It’s about sovereignty. Your neurology deserves more than a pill that passes a regulatory loophole.
Jaswinder Singh
December 7, 2025 AT 10:17Bro I had the same thing happen. Switched to generic lamotrigine, started zoning out, then had a seizure in the shower. My mom found me on the floor. I didn't even feel it coming. After that, I paid out of pocket for the brand. My insurance hated me but my brain is still intact. Stop acting like this is a debate. It's not. It's life or death.
Bee Floyd
December 7, 2025 AT 16:26My cousin’s 12-year-old daughter has Dravet syndrome. She’s on stiripentol-no generic exists. Her family pays $1,200/month. They’ve sold their second car, skipped vacations, and still manage it. But they don’t complain. They just whisper prayers before each dose.
Meanwhile, the rest of us argue over 15% absorption differences.
Let’s not forget: behind every bioequivalence study is a human who just wants to wake up tomorrow without a seizure.
That’s the real metric.
Sean McCarthy
December 8, 2025 AT 19:04Jeremy Butler
December 9, 2025 AT 05:27One must interrogate the ontological presuppositions underpinning the notion of therapeutic equivalence in pharmacological substitution. The Cartesian dualism that separates chemical composition from phenomenological effect is fundamentally flawed. The body does not register milligrams-it registers meaning, rhythm, and continuity. A pill, though chemically identical, is not ontologically identical if its gestalt-its shape, its color, its imprint-has been altered. The psyche, in its somatic entanglement with the pharmacopeia, responds not to molar quantities but to symbolic consistency. To disrupt this is to induce not merely physiological instability, but existential dissonance.
Thus, the question is not whether the generic is bioequivalent, but whether it is *existentially* equivalent. And the answer, empirically and phenomenologically, is: no.
Courtney Co
December 10, 2025 AT 23:19My mom’s on valproate. They switched her to generic. She started forgetting her own name. We thought it was dementia. Turns out, her blood levels dropped 30%. She was lucid for 20 years. Then, one pill changed everything. I called the pharmacy. They said, "It’s FDA-approved." I said, "So was the Titanic."
Don’t tell me it’s safe. I’ve seen what safe looks like after it fails.
Souvik Datta
December 11, 2025 AT 12:28Here’s the truth: medicine is not just chemistry. It’s trust. When you’ve been seizure-free for five years, you don’t just trust the drug-you trust the ritual. The same bottle. The same pill. The same routine. When that changes, even slightly, your brain doesn’t know if it’s safe anymore. And anxiety? It lowers your seizure threshold. So it’s not just the drug. It’s the whole story around it.
That’s why consistency matters. Not because of bioequivalence. Because of human biology. And human hearts.
And yes, I’ve seen people pay extra. I’ve seen them beg doctors to write "do not substitute." I’ve seen them cry because they can’t afford the brand.
So let’s fix the system. Not the patient.
Shashank Vira
December 11, 2025 AT 16:45Let’s not pretend this is about cost. It’s about power. The pharmaceutical industry profits from the brand-name drug, then monopolizes the generic market with identical formulations under a different name. They create the dependency, then sell you the illusion of choice. The FDA’s 80–125% range? A legal loophole designed to maximize shareholder value while minimizing liability. The patients? Disposable variables in a calculus of profit. This isn’t healthcare. It’s a market experiment conducted on vulnerable human beings. And the worst part? We’ve been conditioned to believe this is normal.
Eric Vlach
December 11, 2025 AT 19:31My neuro told me to always check the pill before I take it. Took a pic of my lamotrigine when I started. Now I compare every refill. If it looks different? I call my doctor before I swallow.
It’s not paranoia. It’s just smart.
Also-ask about the fillers. Some generics use lactose. If you’re on keto? That’s a seizure waiting to happen.
And yeah, if you can afford the brand? Do it. If you can’t? Fight for help. The Epilepsy Foundation’s program is real. Ask your doc. Don’t suffer in silence.