Carbamazepine is one of the oldest and most widely used seizure medications, but its hidden power as a drug interaction engine catches many doctors and patients off guard. It doesn’t just treat epilepsy or bipolar disorder-it changes how your body processes almost every other drug you take. If you’re on carbamazepine, or thinking about starting it, you need to know this: it doesn’t just affect you. It affects everything else in your medicine cabinet.
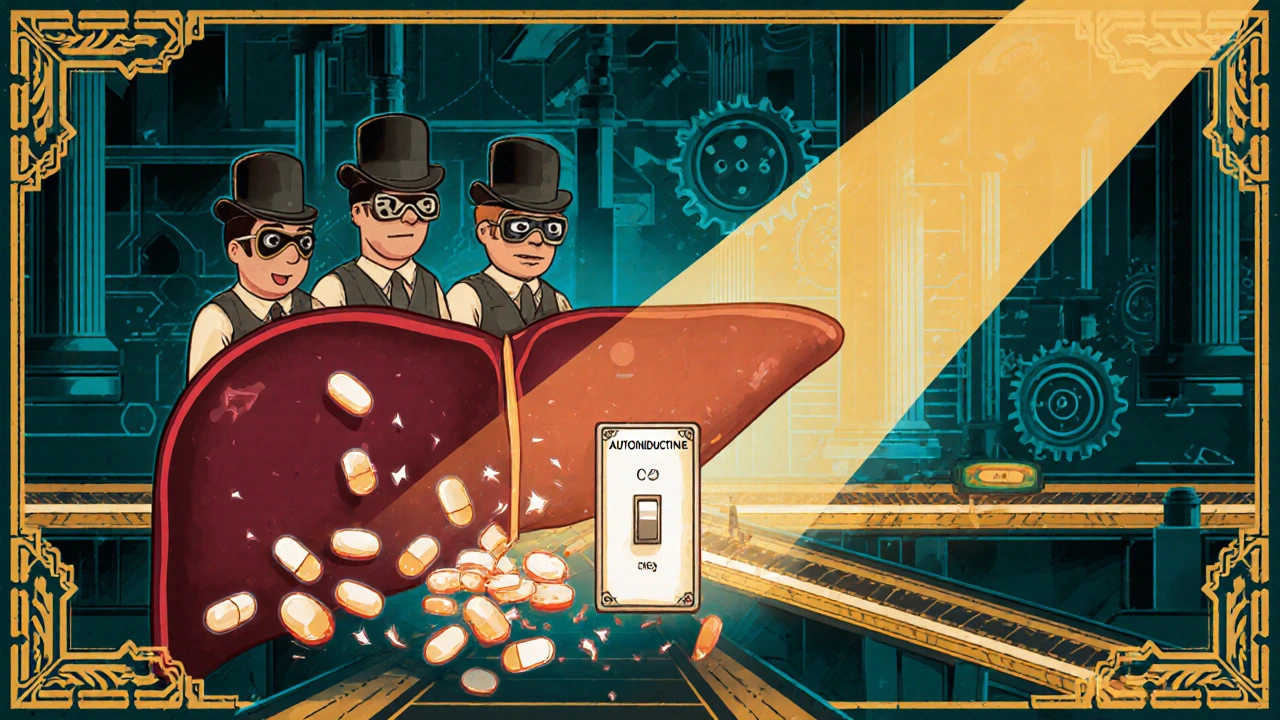
How Carbamazepine Turns Your Liver Into a Drug-Metabolizing Machine
Carbamazepine doesn’t just sit in your system. It wakes up enzymes in your liver-specifically CYP3A4 and CYP2B6-that are responsible for breaking down about half of all prescription drugs. Think of these enzymes as tiny recycling plants. Normally, they work at a steady pace. Carbamazepine flips a switch and turns them into overtime workers. This is called enzyme induction.
The mechanism is surprisingly precise. Carbamazepine binds to nuclear receptors-PXR and CAR-that act like genetic switches. Once activated, these receptors tell your liver to produce more CYP3A4 and CYP2B6 enzymes. The result? Drugs you take get broken down faster, often before they can do their job.
This isn’t theoretical. Studies show carbamazepine can reduce the blood levels of other drugs by 60% to 80%. That’s not a small drop-it’s enough to make a medication useless. And here’s the twist: carbamazepine does this to itself too. That’s called autoinduction. When you start taking it, your body slowly starts breaking it down faster. Within three to four weeks, your carbamazepine levels can drop by 30% to 50%. That’s why many patients have breakthrough seizures in the first month-they’re not getting enough of the drug because their body is learning to destroy it faster.
Drugs That Lose Their Power When Taken With Carbamazepine
Some medications become almost useless when combined with carbamazepine. Here’s what you need to watch out for:
- Oral contraceptives: Ethinyl estradiol levels can drop by 50% to 70%. There are real-world cases of women on birth control pills getting pregnant while taking carbamazepine-even when they never missed a pill.
- Statins: Simvastatin and atorvastatin get broken down so fast that cholesterol control can collapse. One study showed simvastatin’s effectiveness dropped by 74%.
- Warfarin: Your blood thinning effect can vanish. Patients often need to increase their warfarin dose by 50% to 100% just to stay in range. Missing this can lead to strokes or clots.
- Antidepressants: SSRIs like sertraline and SNRIs like venlafaxine lose potency. Some patients report depression returning after carbamazepine is added, even if their epilepsy improves.
- Immunosuppressants: Cyclosporine and tacrolimus levels can plummet, putting transplant patients at risk of organ rejection.
- Benzodiazepines: Alprazolam and clonazepam lose their calming effect. And if you stop carbamazepine suddenly, those same drugs can build up to toxic levels.
These aren’t rare cases. A study of over 2,400 patients found that nearly 4 in 10 needed a dose change because of interactions. The biggest culprits? Blood thinners, antidepressants, and transplant drugs.
Why Carbamazepine Is Different From Other Inducers
There are other strong enzyme inducers-like rifampicin and phenytoin. But carbamazepine has unique traits.
Rifampicin works faster and harder. It can slash drug levels by up to 90%. But it’s not something you take long-term. It’s used for tuberculosis, and its side effects are brutal. Carbamazepine, on the other hand, is taken daily for years. It’s better tolerated, which is why it’s the go-to choice for drug interaction studies. Researchers use it as the gold standard to test how new drugs behave when mixed with strong inducers.
Compared to phenytoin, carbamazepine is more selective. It hits CYP3A4 hard but leaves CYP2C9 mostly alone. That matters because some drugs-like warfarin-are broken down by CYP2C9. Phenytoin can interfere with warfarin more unpredictably. Carbamazepine’s pattern is more consistent, which makes dosing a bit easier to manage.
Still, carbamazepine’s autoinduction makes it a moving target. Rifampicin reaches peak induction in five days. Carbamazepine takes two weeks. And when you stop it? The enzyme levels don’t drop right away. They hang around for weeks. That’s why stopping carbamazepine can be just as dangerous as starting it-if you don’t adjust other meds.

What Happens When You Stop Taking Carbamazepine
Most people focus on the risks of starting carbamazepine. But stopping it is equally tricky.
Once you quit, your liver enzymes don’t turn off overnight. They stay elevated for days or even weeks. That means drugs you were taking before-like alprazolam, cyclosporine, or even some antidepressants-start building up in your blood. You might feel dizzy, drowsy, or nauseous. In severe cases, you could have respiratory depression or kidney toxicity.
Case reports show patients ending up in the ER after stopping carbamazepine because their anxiety meds suddenly became too strong. The fix? Don’t stop carbamazepine cold turkey. And don’t leave other drugs unchanged. Gradually reduce the dose of carbamazepine over two to four weeks. At the same time, lower the doses of any interacting drugs by 25% to 50%. This isn’t optional. It’s life-saving.
Monitoring and Dosing: The Only Reliable Way to Stay Safe
You can’t guess your way out of carbamazepine interactions. You need data.
Therapeutic drug monitoring (TDM) is non-negotiable. Blood tests for carbamazepine levels should be done at baseline, then again at two and four weeks after starting or changing the dose. Why? Because that’s when autoinduction peaks. If your level is below 4 µg/mL, you’re probably not protected from seizures. If it’s above 12 µg/mL, you risk dizziness, double vision, or even liver damage.
But here’s the catch: carbamazepine’s main metabolite-carbamazepine-10,11-epoxide-is also active. Some labs only measure the parent drug. That’s misleading. The metabolite contributes to both effectiveness and side effects. You need to know the total active level.
Doctors should also check for signs of interaction with other drugs. For warfarin, that means frequent INR tests. For birth control, it means switching to a non-hormonal method. For statins, it means switching to pravastatin or rosuvastatin, which aren’t broken down by CYP3A4.
Newer Alternatives and the Future of Treatment
Carbamazepine still has a place. It works well for focal seizures and trigeminal neuralgia. But its interaction profile is a major drawback. That’s why newer drugs are replacing it.
Eslicarbazepine, a cousin of carbamazepine, was designed to be just as effective but with 80% less enzyme induction. Early trials show it doesn’t wreck statins or birth control the same way. It’s not perfect-it still has side effects-but it’s a big step forward.
There’s also research into genetic testing. Some people have variations in their PXR or CAR genes that make them super-inducers. Others barely induce at all. A clinical trial (NCT05678901) is now testing whether we can predict who’ll have bad interactions before they even start carbamazepine. If it works, we could personalize dosing and avoid dangerous surprises.
Meanwhile, extended-release versions like carbamazepine-ASP are being approved. They smooth out blood levels, which may reduce the intensity of autoinduction. Early data suggests they’re less likely to cause sudden drops in other drug levels.
But here’s the reality: carbamazepine isn’t disappearing. It’s too cheap, too effective for certain conditions, and too entrenched in guidelines. That means doctors and patients need to treat it like a nuclear option-not a first-line choice.
What You Should Do Right Now
If you’re on carbamazepine:
- Make a full list of every medication you take-including over-the-counter drugs, supplements, and herbal products.
- Ask your doctor or pharmacist to check for interactions using a reliable tool like Lexicomp or Micromedex.
- Request therapeutic drug monitoring if you haven’t had it in the last month.
- If you’re on birth control, switch to an IUD or implant. Pills won’t work.
- If you’re on warfarin, get your INR checked weekly for the first month after starting carbamazepine.
- If you’re thinking of stopping carbamazepine, don’t do it without a plan. Talk to your doctor about tapering and adjusting other meds.
If you’re a clinician: don’t assume your patient knows about these interactions. Many don’t. Write clear instructions. Use checklists. Track changes. Carbamazepine isn’t just a seizure drug. It’s a pharmacokinetic wildcard. Treat it like one.
Can carbamazepine cause birth control to fail?
Yes. Carbamazepine can reduce the effectiveness of hormonal birth control by 50% to 70%. This isn’t a rare side effect-it’s well-documented. Women taking carbamazepine who rely on pills, patches, or rings have a significantly higher risk of unintended pregnancy. The only safe options are non-hormonal methods like copper IUDs, barrier methods, or sterilization.
How long does it take for carbamazepine to start inducing enzymes?
It takes about 10 to 14 days for carbamazepine to fully induce CYP3A4 and CYP2B6 enzymes. This is why patients often don’t notice problems right away. But autoinduction-where carbamazepine speeds up its own metabolism-starts within days and peaks around 3 to 4 weeks. That’s why blood levels drop even if the dose stays the same.
Is carbamazepine still used today, or are there better options?
Yes, carbamazepine is still widely used, especially for focal seizures and trigeminal neuralgia. It’s inexpensive and effective. But because of its strong interaction profile, it’s no longer a first choice for bipolar disorder or new epilepsy patients. Newer drugs like eslicarbazepine, lamotrigine, and levetiracetam are preferred because they don’t trigger major drug interactions. Carbamazepine remains essential-but only when safer options won’t work.
What should I do if I need to stop taking carbamazepine?
Never stop abruptly. Taper the dose slowly over 2 to 4 weeks under medical supervision. At the same time, reduce the doses of any other drugs metabolized by CYP3A4 or CYP2B6-like alprazolam, cyclosporine, or simvastatin-by 25% to 50%. Otherwise, those drugs can build up to toxic levels, causing drowsiness, confusion, or organ damage.
Can I take over-the-counter supplements with carbamazepine?
Many supplements can interact. St. John’s wort is a strong CYP3A4 inducer and can make carbamazepine less effective. Garlic, grapefruit juice, and milk thistle can also interfere with liver enzymes. Even common vitamins like vitamin D and calcium can affect absorption. Always check with your pharmacist before starting any supplement.

Chrisna Bronkhorst
November 14, 2025 AT 10:07Andrew Forthmuller
November 14, 2025 AT 14:43Danae Miley
November 14, 2025 AT 18:53Charles Lewis
November 16, 2025 AT 17:37Eve Miller
November 17, 2025 AT 23:32Renee Ruth
November 18, 2025 AT 23:51Samantha Wade
November 20, 2025 AT 19:24Elizabeth Buján
November 21, 2025 AT 02:52vanessa k
November 22, 2025 AT 15:55