Clarithromycin Drug Interaction Checker
Check for Dangerous Interactions
Enter the medications you're currently taking. This tool identifies dangerous combinations with clarithromycin based on FDA warnings and medical research.
Interaction Results
Risk assessment: No dangerous interactions detected
Dangers Identified
Recommended Actions
WARNING: Immediate medical attention required
If you have taken clarithromycin with any of these medications, stop the antibiotic immediately (if less than 48 hours) and contact your doctor or go to the emergency room if you experience:
- Muscle pain or weakness
- Dark urine
- Nausea or vomiting
- Irregular heartbeat
- Confusion or dizziness
Clarithromycin is a powerful antibiotic used to treat infections like pneumonia, bronchitis, and skin infections. But for many people, taking it can be dangerous - not because of the infection it’s meant to fight, but because of what it does to other medications already in your system. This isn’t a rare side effect. It’s a well-documented, life-threatening risk that happens more often than most doctors and patients realize.
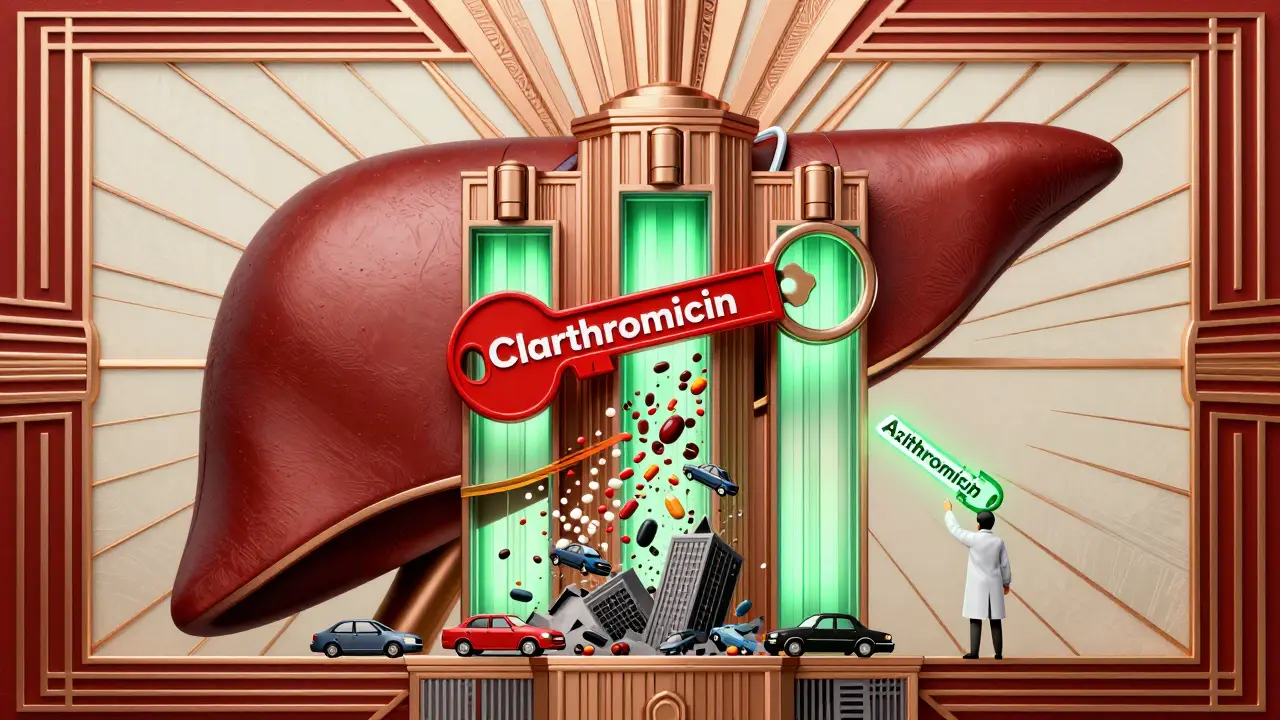
Why Clarithromycin Is Riskier Than Other Antibiotics
Clarithromycin doesn’t just kill bacteria. It also shuts down a key liver enzyme called CYP3A4. This enzyme is responsible for breaking down about half of all prescription drugs. When clarithromycin blocks it, those drugs build up in your blood to toxic levels. That’s why even a normal dose of another medication can become deadly when taken with clarithromycin.
Compare this to azithromycin, another macrolide antibiotic. Azithromycin barely touches CYP3A4. That’s why doctors now prefer it for most patients - especially those on multiple medications. A 2018 study found clarithromycin was 2.8 times more likely to cause serious drug interactions than azithromycin. And it’s not just a theory. Real patients have died from this.
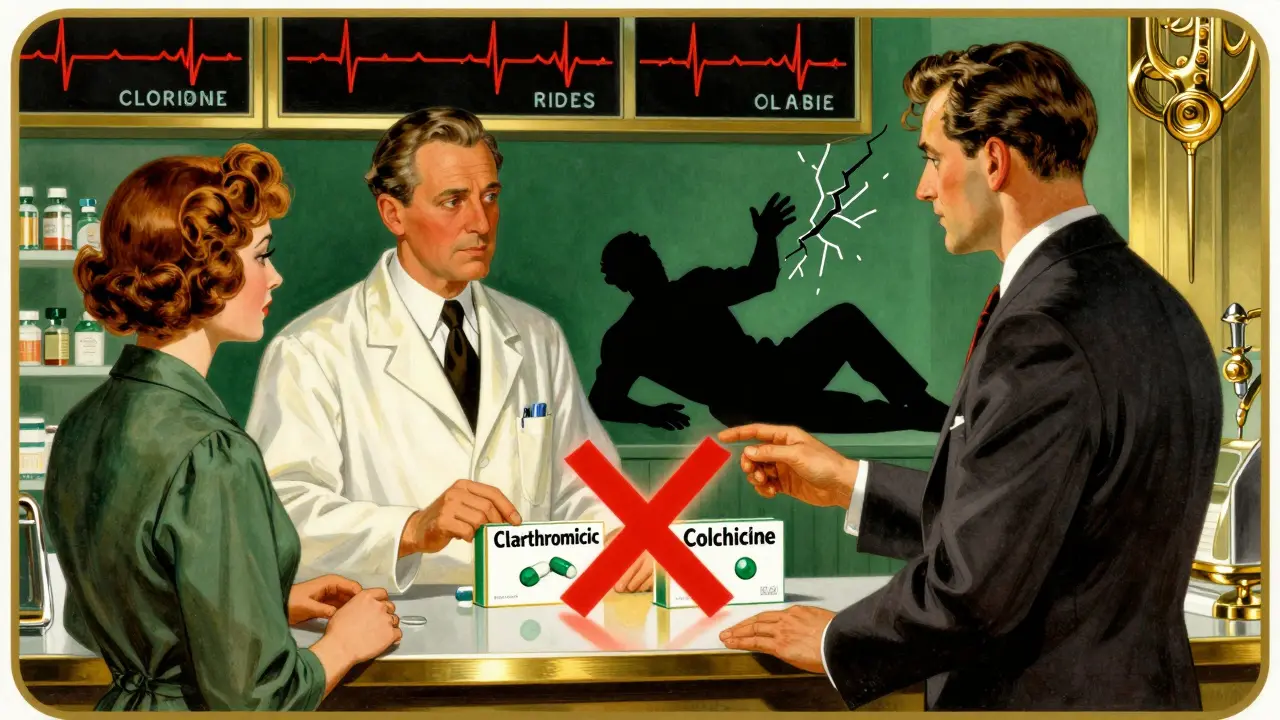
The Deadliest Combo: Clarithromycin and Colchicine
If you take colchicine for gout, clarithromycin could kill you. This isn’t a hypothetical warning. The FDA has documented 58 serious or fatal cases of this interaction as of 2020. Many ended in death within two weeks.
Colchicine is normally safe at low doses. But when clarithromycin blocks its breakdown, blood levels can spike by more than 280%. That’s enough to cause severe diarrhea, muscle damage, kidney failure, and multi-organ shutdown. One case involved a 76-year-old woman with chronic gout who started clarithromycin for a cough. She died 11 days later. Her colchicine dose hadn’t changed - but the antibiotic turned it into poison.
The Institute for Safe Medication Practices calls this a Category A high-alert interaction - the highest risk category. That means if a pharmacist spots this combo, they’re legally required to stop it.
Statins: The Silent Killer
Many people take statins like simvastatin or lovastatin to lower cholesterol. These drugs are already known to cause muscle damage. But add clarithromycin, and that risk skyrockets.
A 68-year-old man taking 40mg of simvastatin daily was prescribed clarithromycin for a sinus infection. Within 72 hours, he developed rhabdomyolysis - a condition where muscle tissue breaks down and floods the bloodstream with toxins. He ended up in the ICU and needed dialysis. His liver enzymes were through the roof. His kidneys were failing. He survived - but barely.
Atorvastatin is less risky than simvastatin, but it’s still dangerous with clarithromycin. The Mayo Clinic lists all three statins as absolute no-gos with clarithromycin. If you’re on any statin, ask your doctor to switch you to a different antibiotic - or switch your statin to one that doesn’t rely on CYP3A4, like pravastatin or rosuvastatin.
Heart Medications: A Recipe for Cardiac Arrest
Clarithromycin doesn’t just interfere with metabolism. It also prolongs the QT interval - the time your heart takes to recharge between beats. When combined with other QT-prolonging drugs, it can trigger a deadly heart rhythm called torsades de pointes.
Calcium channel blockers like verapamil, diltiazem, and amlodipine are common for high blood pressure and angina. But with clarithromycin, they can cause dangerously low blood pressure or heart block. Antiarrhythmics like amiodarone and quinidine are even worse. The American Heart Association says clarithromycin triples the risk of torsades compared to safer antibiotics.
One study found that patients taking clarithromycin with a QT-prolonging drug had a 2.7-fold higher chance of sudden cardiac death. That’s not a small risk. That’s a red flag.
Other Dangerous Interactions
Clarithromycin doesn’t stop at statins and heart drugs. It can turn common medications into hazards:
- Digoxin: Levels can double, leading to nausea, confusion, and fatal heart rhythms.
- Warfarin: Increased bleeding risk due to reduced metabolism - INR levels can spike unpredictably.
- Theophylline: Used for asthma, this drug can build up to toxic levels, causing seizures or heart arrhythmias.
- Ergotamine: Used for migraines, this can cause limb ischemia - tissue death from lack of blood flow.
- Rivaroxaban and other blood thinners: Increased bleeding risk, especially in older adults.
The Mayo Clinic’s interaction checker flags 142 drugs as contraindicated with clarithromycin. That’s more than most people take in a lifetime. And if you’re over 65? The risk is even higher. Studies show 42% of older adults on clarithromycin are also taking at least one dangerous drug.
What Should You Do?
If your doctor prescribes clarithromycin, ask these questions right away:
- Am I taking any statins? If yes, which one?
- Do I take colchicine for gout?
- Am I on any blood pressure or heart rhythm medications?
- Do I take warfarin, digoxin, or any seizure or migraine drugs?
If you answer yes to any of these, push for an alternative. Azithromycin is almost always a safer choice. It’s just as effective for most infections - and doesn’t mess with your other meds.
If clarithromycin is absolutely necessary - say, for a stubborn Mycobacterium avium infection - your doctor should:
- Stop the interacting drug for the duration of treatment
- Reduce the dose of the interacting drug by 50-75%
- Monitor blood levels if possible (especially for digoxin or theophylline)
- Watch for signs of toxicity: muscle pain, weakness, nausea, irregular heartbeat, confusion
Why Is This Still Happening?
Despite all the warnings, clarithromycin is still prescribed. Why? Because it works well against certain bacteria. But that’s not enough. The FDA added a boxed warning in 2023 - the strongest possible alert - specifically for the colchicine interaction. The European Medicines Agency has banned it in patients with kidney problems who take colchicine. The American College of Physicians now recommends azithromycin as the default macrolide for anyone on three or more medications.
Prescriptions for clarithromycin have dropped 28% since 2015. Azithromycin now makes up 63% of all macrolide prescriptions in the U.S. Doctors are switching - not because azithromycin is stronger, but because it’s safer.
If your doctor says, ‘It’s fine, I’ve prescribed this before,’ ask: ‘Have any of your patients had a bad reaction?’ Chances are, they haven’t asked the question themselves.
What to Do If You’ve Already Taken Both
If you’ve taken clarithromycin with colchicine, simvastatin, or another high-risk drug:
- Stop the antibiotic immediately - but only if you’ve been on it less than 48 hours
- Call your doctor or go to the ER if you have muscle pain, weakness, dark urine, nausea, vomiting, or irregular heartbeat
- Don’t wait for symptoms to get worse. Toxicity can hit fast - sometimes within 24 hours
- Bring a full list of all your medications to the hospital
There’s no antidote. Treatment is supportive: fluids, kidney support, stopping the drugs, and monitoring heart rhythm. Survival depends on how fast you act.
The Bottom Line
Clarithromycin isn’t evil. It saves lives. But it’s not a first-choice antibiotic anymore - not when safer options exist. For most infections, azithromycin, amoxicillin, or doxycycline work just as well without the risk.
If you’re on multiple medications - especially if you’re over 65 - never start clarithromycin without checking every single drug you take. Your pharmacist can run the interaction check in seconds. Use them. Ask them. Demand it.
There’s no shame in asking for a different antibiotic. There’s only shame in letting a preventable death happen because no one asked the right question.
Can I take clarithromycin if I have gout and take colchicine?
No. Taking clarithromycin with colchicine can cause fatal toxicity. Even a normal dose of colchicine can become deadly. The FDA has issued a boxed warning for this combination. Always tell your doctor you take colchicine before starting any antibiotic. Switch to azithromycin instead.
Is azithromycin safer than clarithromycin?
Yes. Azithromycin has minimal effect on the CYP3A4 enzyme, meaning it rarely causes dangerous drug interactions. It’s just as effective as clarithromycin for most common infections like sinusitis, bronchitis, and pneumonia. For patients on multiple medications, especially older adults, azithromycin is now the preferred macrolide.
What statins are dangerous with clarithromycin?
Simvastatin and lovastatin are the most dangerous. Atorvastatin is also risky. These statins are broken down by CYP3A4, and clarithromycin blocks that process, leading to muscle damage and rhabdomyolysis. Safer alternatives include pravastatin, rosuvastatin, or fluvastatin, which use different metabolic pathways.
Can I take clarithromycin if I’m on blood pressure medication?
It depends. Calcium channel blockers like verapamil, diltiazem, and amlodipine can become dangerously potent when combined with clarithromycin, leading to low blood pressure or heart block. If you take one of these, ask for azithromycin or another antibiotic. Never assume it’s safe just because your blood pressure seems stable.
How long does clarithromycin affect drug metabolism?
Clarithromycin’s effect on CYP3A4 can last for several days after you stop taking it. Even if you finish your course, you should wait at least 5-7 days before restarting any interacting medication. For high-risk drugs like colchicine or statins, your doctor may recommend a longer gap or a temporary switch to a safer alternative.
Always review your full medication list with your pharmacist before starting any new antibiotic. A quick check takes 30 seconds - and could save your life.


Sangeeta Isaac
January 19, 2026 AT 14:15so i took clarithromycin last year for a sinus infection and didn't think twice... turns out i was on simvastatin. i got this weird muscle ache that felt like i'd been hit by a truck for a week. doc said 'probably just sore from coughing.' yeah right. i'm never trusting a script without checking with my pharmacist again. 🙃
Alex Carletti Gouvea
January 20, 2026 AT 22:40why are we letting big pharma dictate what antibiotics we use? clarithromycin works. people have been taking it for decades. if you're dumb enough to mix it with statins or colchicine, that's on you. stop blaming the drug.
Philip Williams
January 21, 2026 AT 16:38This is an exceptionally well-documented and clinically vital post. The CYP3A4 inhibition mechanism is not merely theoretical-it is empirically validated across multiple peer-reviewed studies, including those published in JAMA and the New England Journal of Medicine. The FDA’s boxed warning for colchicine interactions is not a suggestion; it is a legal and ethical imperative. I urge all clinicians to adopt azithromycin as the default macrolide in polypharmacy patients, particularly those over 65. Pharmacist-led medication reconciliation should be standard protocol, not an afterthought.
Ben McKibbin
January 21, 2026 AT 16:51Can we talk about how absurd it is that we still have to beg doctors to check interactions? I had my pharmacist flag clarithromycin + amlodipine last month. The prescriber said, 'Oh, I’ve done this a hundred times.' My pharmacist said, 'And how many of those patients ended up in the ER?' Silence. Then the script got changed. We need mandatory interaction checks built into EHRs-like, yesterday. This isn’t ‘medical nuance,’ it’s preventable death by paperwork negligence.
Uju Megafu
January 22, 2026 AT 07:31OH MY GOD I KNEW IT. I TOLD MY MOM NOT TO TAKE THAT ANTIBIOTIC BUT SHE SAID 'THE DOCTOR KNOWS BEST' AND NOW SHE'S IN THE HOSPITAL WITH RENAL FAILURE AND HER KNEES ARE SWOLLEN LIKE BALLOONS. I TOLD YOU ALL. I TOLD YOU. THIS IS WHY I DON'T TRUST DOCTORS. THEY'RE ALL JUST MONEY-DRIVEN ROBOTS. CLARITHROMYCIN IS A WEAPON. THEY KNOW. THEY KNOW AND THEY STILL PRESCRIBE IT. #FREEDOMFROMPHARMA
Amber Lane
January 23, 2026 AT 13:01My grandma took clarithromycin and died. She was on colchicine. No one asked. No one checked. I still cry when I think about it.
Ashok Sakra
January 25, 2026 AT 07:59bro why u even take medicine? just eat garlic and pray. i took clarithromycin and i feel fine. u just scared of pills.
Andrew Rinaldi
January 26, 2026 AT 02:37It’s fascinating how medical knowledge evolves. We used to think antibiotics were just about killing bugs. Now we see they’re more like conductors in an orchestra of metabolism. One wrong note-and the whole system collapses. Clarithromycin isn’t evil. It’s just… loud. And we’re finally learning to turn down the volume.
Gerard Jordan
January 27, 2026 AT 03:32Just had my pharmacist pull me aside after I got a clarithromycin script. She said, 'Let me guess-you're on Lipitor?' Yep. She swapped it for azithromycin on the spot. 🙏 I didn't even ask. She just… knew. Pharmacist heroes. Real ones. 🏥💖 #ThankYouPharmacists
michelle Brownsea
January 28, 2026 AT 04:23Let me be absolutely clear: This is not ‘a risk.’ This is a catastrophic, preventable, systemic failure of medical education, pharmaceutical oversight, and physician accountability. The fact that this interaction is still occurring in 2025-despite FDA warnings, EMA bans, and ACP guidelines-is not negligence. It is malpractice. And if your doctor prescribes clarithromycin without reviewing your entire medication list, they are not your doctor-they are a liability.
Roisin Kelly
January 28, 2026 AT 04:47They’re all lying. Clarithromycin is just the tip of the iceberg. The real agenda? Make us dependent on meds so they can sell us more. They don’t want us healthy-they want us hooked. I stopped all my meds after this. Now I drink lemon water and ‘vibrate at a higher frequency.’ My cholesterol’s higher but my soul? Free.
lokesh prasanth
January 28, 2026 AT 14:44azithromycin good. clarithromycin bad. why still use? dumb doctors. my uncle died. no one check. same story everywhere.