Decongestant Safety Checker
Check Your Decongestant Safety
Enter your blood pressure and medication information to see if decongestants are safe for you.
Many people reach for decongestants when they have a cold or allergies. It’s quick, easy, and available right on the shelf. But if you have high blood pressure, that little bottle might be hiding a serious risk. You might not realize it, but decongestants can push your blood pressure higher - sometimes dangerously so - and interfere with the very medications you take to keep it under control.
How Decongestants Work (and Why That’s a Problem)
Decongestants like pseudoephedrine and phenylephrine work by tightening blood vessels in your nose. That reduces swelling and lets you breathe easier. But here’s the catch: they don’t just tighten vessels in your nose. They tighten blood vessels everywhere - including those that carry blood to your heart and brain. This forces your heart to pump harder, raising your blood pressure.
It’s not a small effect. Studies show that pseudoephedrine, the most common decongestant in cold medicines, can raise systolic blood pressure by 3 to 5 mm Hg on average. For someone with controlled hypertension, that might seem minor. But for someone with uncontrolled high blood pressure, it can be enough to trigger a spike that leads to headaches, dizziness, or worse. In rare cases, it’s been linked to heart attacks, strokes, and irregular heart rhythms.
Phenylephrine, which replaced pseudoephedrine in many OTC products after 2020, was thought to be safer. But newer research shows it has similar effects. A 2023 study in US Pharmacist found that even low doses of phenylephrine, taken over several days, could push a child’s blood pressure into the hypertensive range. That’s not a fluke - it’s a pattern.
Who’s at the Highest Risk?
Not everyone with high blood pressure will have a bad reaction. But some people are far more vulnerable:
- Those with uncontrolled hypertension - blood pressure consistently above 140/90
- People with heart disease, including prior heart attacks or heart failure
- Those with arrhythmias or a history of irregular heartbeats
- Patients with Prinzmetal angina - a rare form of chest pain caused by artery spasms
- Anyone taking MAO inhibitors (like Nardil or Parnate) or certain antidepressants
The risk isn’t just about the decongestant itself. It’s about what else is in your system. Some blood pressure medications - especially beta-blockers and diuretics - can interact poorly with decongestants, making the rise in pressure worse. And if you’re taking multiple prescriptions, the chance of a hidden interaction goes up.
Where Decongestants Hide (And Why You’re Probably Taking Them Without Knowing)
Most people think they’re just taking a cold tablet. But decongestants are often hidden in multi-symptom products. You might not even realize you’re taking one.
Here are common OTC products that contain decongestants:
- Tylenol Cold and Flu
- Advil Multi-Symptom Cold and Flu
- Benadryl Allergy Plus Congestion
- Mucinex Sinus Max
- Robitussin Cold & Flu
- DayQuil and NyQuil (many versions)
Even if you’re careful about your blood pressure meds, you might grab one of these because it says "allergy relief" or "sinus relief." The label doesn’t scream "dangerous." But the ingredient list does. Look for these names:
- Pseudoephedrine
- Phenylephrine
- Ephedrine
- Naphazoline
- Oxymetazoline
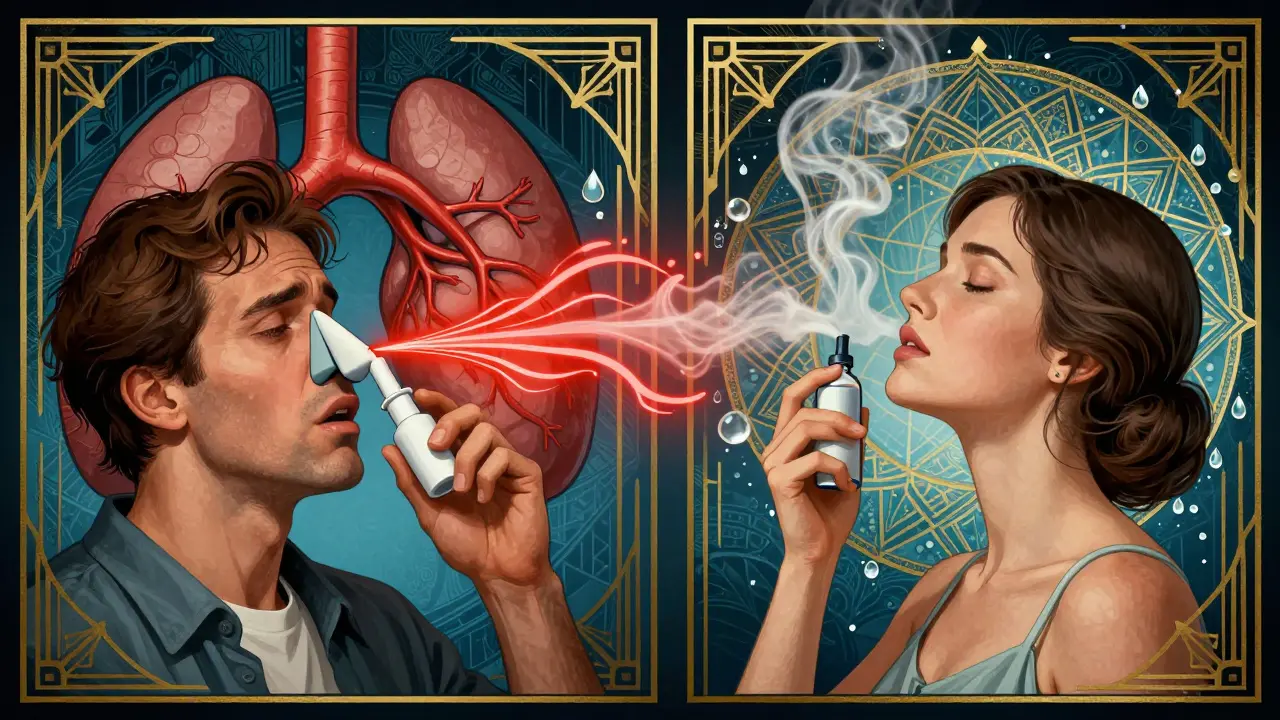
And don’t forget nasal sprays. Products like Afrin (oxymetazoline) can cause the same problem - even if you’re only using them in your nose. They’re absorbed into your bloodstream. One study found that regular use of nasal decongestant sprays led to sustained increases in blood pressure in hypertensive patients.
What the Experts Say
The American Heart Association is clear: if you have high blood pressure, avoid decongestants unless your doctor says it’s okay. The Mayo Clinic goes further - they advise people with severe or uncontrolled hypertension to avoid them entirely.
Harvard Health says that even if your blood pressure is well-controlled, you should still check with your doctor first. Why? Because everyone reacts differently. One person might take a single dose and feel fine. Another might see their pressure jump 20 points. There’s no way to predict it.
Pharmacists in the UK and US now spend 3 to 5 minutes per customer during cold season just explaining these risks. That’s because so many people don’t know. A 2023 survey found that nearly 1 in 6 hypertensive patients had taken a decongestant in the past year - despite knowing they had high blood pressure.
Safe Alternatives for Nasal Congestion
You don’t have to suffer through a stuffy nose. There are safer ways to clear your sinuses:
- Saline nasal spray - no drugs, no side effects. Just salt water. Use it 2-3 times a day.
- Steam inhalation - breathe in warm steam from a bowl of hot water (add a drop of eucalyptus oil if you like). Cover your head with a towel and inhale for 5-10 minutes.
- Humidifier - keeping the air moist helps reduce swelling in nasal passages.
- Antihistamines without decongestants - like loratadine (Claritin) or cetirizine (Zyrtec). These help with allergies but don’t raise blood pressure.
- Neti pot - rinsing your nasal passages with sterile saline can clear congestion naturally.
Even these alternatives aren’t risk-free. If you have asthma or chronic sinus issues, talk to your doctor before trying anything new.
What to Do Right Now
If you have high blood pressure, here’s your action plan:
- Check every medicine you take - including OTC, herbal, and supplements. Look for decongestant ingredients.
- Ask your pharmacist - they’re trained to spot these interactions. Don’t be shy. Say, "I have high blood pressure - is this safe?"
- Monitor your blood pressure - if you’ve taken a decongestant recently, check your pressure at home for the next 48 hours.
- Don’t assume "natural" means safe - some herbal cold remedies contain ephedra or other stimulants that are even riskier.
- Keep a list - write down all your medications and share it with your doctor at every visit.
It’s easy to think, "It’s just a cold medicine." But for someone with high blood pressure, it’s not just a cold medicine. It’s a potential trigger for something much worse.
Why This Matters More Than Ever
More people than ever are living with high blood pressure. In the UK alone, over 10 million adults have diagnosed hypertension. And that number is rising. At the same time, multi-symptom cold products are becoming more common - packed with more ingredients, more convenience, and more hidden risks.
The warning labels have changed. They used to say "Do not use if you have high blood pressure." Now they say, "Ask your doctor before use." That shift tells you everything. It’s no longer black and white. It’s about your personal health picture.
What’s safe for your neighbor might not be safe for you. And the only way to know is to ask - before you take it.

