Herbal Tea-Medication Interaction Checker
Many people drink herbal teas thinking they’re harmless-just a warm, natural way to relax or feel better. But if you’re taking prescription medications, that cup of chamomile or hibiscus tea might be doing more than soothing your throat. It could be interfering with how your drugs work, sometimes in dangerous ways.
Why Herbal Teas Aren’t Just ‘Natural’ Drinks
Herbal teas aren’t tea in the traditional sense. They don’t come from the Camellia sinensis plant. Instead, they’re made from roots, flowers, seeds, or leaves of other plants-like chamomile, peppermint, ginger, or hibiscus. People use them for sleep, digestion, colds, or even to lower blood pressure. But unlike pharmaceuticals, these teas aren’t tested for safety before they hit store shelves. The FDA treats them as food, not medicine. That means no required clinical trials, no standardized dosing, and no warning labels about interactions.That’s a problem when you’re on medication. Even something as simple as three cups of strong green tea a day can cut the effectiveness of your beta-blocker by 85%. That’s not a theory. That’s what a 2023 clinical trial showed in 12 people taking nadolol. The same study found green tea reduced atorvastatin levels by up to 39%. If you’re on these drugs, that’s not just a minor tweak-it could mean your heart condition isn’t controlled, or your cholesterol is rising without you knowing.
Green Tea: The Silent Drug Thief
Green tea is one of the most popular herbal drinks in the U.S. But its active compound, epigallocatechin gallate (EGCG), doesn’t just fight free radicals. It also blocks the transporters your body uses to absorb certain drugs. Specifically, it shuts down OATP1A1 and OATP1A2-proteins that move statins, beta-blockers, and even some antibiotics into your bloodstream.That’s why people taking atorvastatin (Lipitor), nadolol (Corgard), or fluoroquinolone antibiotics like ciprofloxacin may see their drug levels drop dramatically. In lab studies, green tea extract made simvastatin concentrations jump by more than double. That sounds good, right? But too much simvastatin can cause muscle damage. The body doesn’t always balance this out. And because green tea is sold as a tea, not a supplement, most people don’t realize they’re consuming a potent bioactive compound.
If you’re on any of these medications, don’t assume one cup a day is safe. Strong brews, daily use, and concentrated extracts all raise the risk. Even if you feel fine, your blood levels could be dangerously low-or high.
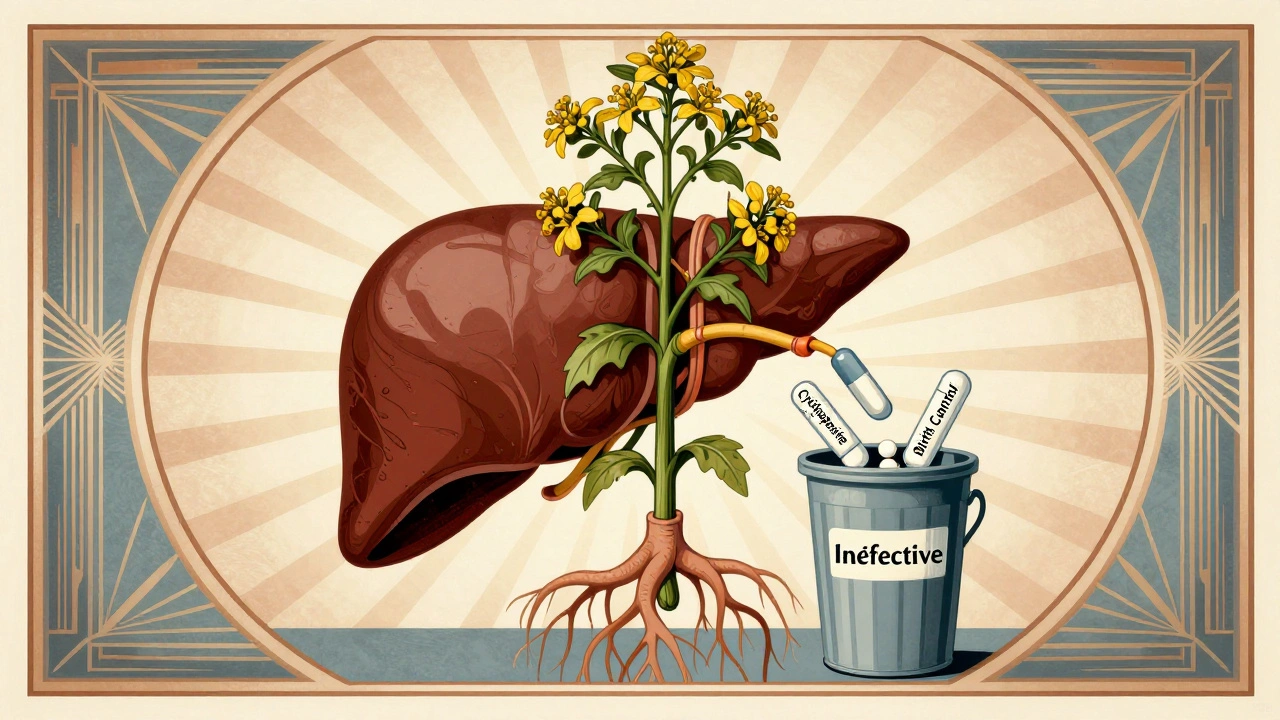
St. John’s Wort and the Hidden Drug Killer
St. John’s wort is often promoted for mild depression. But it’s not harmless. It turns on an enzyme in your liver called CYP3A4. This enzyme breaks down drugs faster. The result? Your medication gets flushed out before it can do its job.This isn’t theoretical. People on cyclosporine (used after transplants) have rejected their new organs because St. John’s wort lowered drug levels. Those on birth control pills have gotten pregnant. People on antidepressants like SSRIs have developed serotonin syndrome-a life-threatening condition caused by too much serotonin in the brain.
The National Center for Complementary and Integrative Health says St. John’s wort affects over 50 drugs. That includes blood thinners, HIV meds, cancer treatments, and even some heart medications. And because it’s sold as a tea or capsule labeled “natural,” many people never tell their doctor they’re taking it. One study found only 25% of older adults who use herbal supplements mention them to their provider.

Chamomile, Hibiscus, and Blood Pressure Risks
Chamomile tea is calming. Hibiscus tea is tart and popular for lowering blood pressure. But if you’re already on a blood pressure pill like lisinopril or losartan, combining it with hibiscus tea can push your pressure too low. There are documented cases where systolic blood pressure dropped below 90 mmHg-enough to cause dizziness, fainting, or even falls.Chamomile contains apigenin, which may interfere with how your liver processes drugs. Early studies suggest it could reduce the effectiveness of oral contraceptives. While more research is needed, the risk isn’t zero. And if you’re taking a pill that needs to stay at a precise level-like birth control-any reduction could have real consequences.
Even something as common as licorice root tea can be risky. It lowers potassium levels. If you’re on diuretics or heart medications, that can trigger irregular heart rhythms. The American Heart Association warns against combining potassium-lowering herbs with heart drugs.
Warfarin and the Bleeding Danger Zone
Warfarin is one of the most dangerous drugs to mix with herbal teas. It’s a blood thinner with a narrow window: too little, and you risk a clot; too much, and you bleed internally. Ginkgo biloba, garlic, ginger, and even chamomile can increase bleeding risk when taken with warfarin.Here’s the twist: cranberry tea is often blamed for raising INR levels (a measure of blood clotting time). But studies are mixed. Some show a clear effect. Others show nothing. That uncertainty makes it even more dangerous. You can’t rely on anecdotal advice. If you’re on warfarin, avoid ginkgo, ginseng, and high-dose ginger teas entirely. And if you’re drinking cranberry tea regularly, get your INR checked more often.
Goldenseal, sometimes brewed as a tea for colds, is another red flag. It blocks the CYP2D6 and CYP3A4 enzymes-enzymes that process over half of all prescription drugs. That includes painkillers, antidepressants, and even some chemotherapy agents.
What You Should Do Right Now
If you take any prescription medication, here’s what to do:- Make a list of every herbal tea you drink, how often, and how strong. Include blends-many contain multiple herbs.
- Bring it to your next doctor’s visit. Don’t wait for them to ask. Say, “I drink chamomile tea every night and hibiscus tea in the morning. Should I be worried?”
- Avoid concentrated extracts. A tea bag is one thing. A capsule labeled “1000mg hibiscus extract” is another. Extracts are far more potent and risky.
- Don’t assume safety. Just because something is sold in a grocery store doesn’t mean it’s safe with your meds.
- Watch for warning signs: Unexplained bruising, dizziness, irregular heartbeat, sudden fatigue, or changes in mood. These could signal an interaction.
Who’s Most at Risk?
Older adults are the most vulnerable. They’re more likely to take multiple medications-and more likely to use herbal teas for arthritis, sleep, or digestion. But they’re also less likely to tell their doctor. Polypharmacy (taking five or more drugs) multiplies the risk. A single herb can interact with multiple medications at once.People with chronic conditions-heart disease, diabetes, epilepsy, or autoimmune disorders-are also at higher risk. Their drugs often have narrow therapeutic windows. Even small changes in drug levels can lead to hospitalization.
And don’t think it’s just seniors. Younger people on birth control, antidepressants, or thyroid meds are just as vulnerable. The rise of “functional teas” marketed for energy, sleep, or immunity means more people are consuming herbal blends without knowing what’s in them.
The Bottom Line
Herbal teas aren’t inherently bad. But they’re not harmless either. They’re powerful plant extracts with real chemical effects on your body. When combined with medications, those effects can become unpredictable-and sometimes deadly.There’s no blanket rule. Some teas are safe. Others aren’t. The only way to know for sure is to talk to your doctor or pharmacist-and show them exactly what you’re drinking. Don’t rely on internet forums or supplement labels. Your health isn’t a guess. It’s a calculation. And you need the right data to make it work.
If you’re taking warfarin, digoxin, cyclosporine, theophylline, or any heart, thyroid, or psychiatric medication-err on the side of caution. Skip the herbal teas until you’ve had a conversation with your provider. It’s not about giving up comfort. It’s about staying safe.
Can I still drink herbal tea if I’m on medication?
Maybe-but not without checking. Some herbal teas are safe with certain meds, while others can be dangerous. Green tea can reduce the effectiveness of beta-blockers and statins. St. John’s wort can make antidepressants, birth control, and transplant drugs stop working. Chamomile and hibiscus may interfere with blood pressure medications. The safest approach is to tell your doctor or pharmacist exactly what teas you drink and ask if they’re safe with your prescriptions.
Is green tea safe with blood pressure medicine?
It depends. Green tea can lower blood pressure on its own, which might sound helpful. But if you’re already on a blood pressure pill like lisinopril or metoprolol, combining it with green tea can push your pressure too low. In one study, people taking nadolol saw an 85% drop in drug levels after drinking three cups of strong green tea daily. That’s not just a minor interaction-it can leave your heart unprotected. If you’re on beta-blockers or statins, limit green tea to one weak cup a day or avoid it entirely until you’ve spoken to your doctor.
Does chamomile tea affect birth control?
There’s evidence it might. Chamomile contains apigenin, which may interfere with liver enzymes that process hormones in birth control pills. While no large human trials have confirmed this, case reports and lab studies suggest a possible risk. If you’re relying on birth control for pregnancy prevention, it’s not worth the gamble. Switch to caffeine-free black or rooibos tea instead, or ask your doctor if your current tea is safe.
Can herbal teas cause bleeding?
Yes. Several herbs-including ginkgo, garlic, ginger, ginseng, and chamomile-can thin the blood. When taken with warfarin, aspirin, or other blood thinners, they increase the risk of internal bleeding, bruising, or stroke. Even a daily cup of ginger tea can raise your INR levels. If you’re on anticoagulants, avoid these herbs completely. The FDA warns that combining these with blood thinners can increase the risk of bleeding or stroke.
Why don’t herbal tea labels warn about drug interactions?
Because the FDA doesn’t require it. Under the Dietary Supplement Health and Education Act of 1994, herbal teas are regulated as food, not drugs. That means manufacturers don’t need to prove safety or effectiveness before selling them. They also don’t need to list potential drug interactions on the label. The FDA only steps in after someone gets hurt. That’s why it’s up to you to ask your doctor about what you’re drinking-even if it’s labeled “natural” or “organic.”
What’s the safest herbal tea to drink with meds?
Rooibos tea is generally considered the safest option. It’s naturally caffeine-free, doesn’t contain compounds known to interfere with liver enzymes or drug transporters, and has no documented interactions with common medications. Peppermint tea is also low-risk for most people, though it can affect stomach acid and may interfere with some acid-reducing drugs. If you’re unsure, stick with plain rooibos or ask your pharmacist. When in doubt, skip the herbal blends and choose single-ingredient teas you can research.
What to Do Next
If you’re on medication and drink herbal teas, don’t wait for a problem to happen. Take action now:- Write down every herbal tea you drink-even if you only have it once a week.
- Bring that list to your next appointment. Show it to your doctor or pharmacist.
- Ask: “Could any of these interfere with my medications?”
- If you’re on warfarin, digoxin, cyclosporine, or thyroid meds, avoid all herbal teas until you’ve had this conversation.
- When in doubt, choose rooibos or plain hot water with lemon.
Your health isn’t a gamble. Herbal teas can be part of a healthy routine-but only if you know how they play with your meds. Don’t assume safety. Ask. Check. Confirm. It’s the only way to stay protected.


Mellissa Landrum
December 5, 2025 AT 19:39Mark Curry
December 6, 2025 AT 03:02Manish Shankar
December 6, 2025 AT 17:52luke newton
December 8, 2025 AT 07:50an mo
December 9, 2025 AT 14:27aditya dixit
December 9, 2025 AT 15:47Mark Ziegenbein
December 11, 2025 AT 14:10Juliet Morgan
December 12, 2025 AT 05:01Deborah Jacobs
December 13, 2025 AT 04:50James Moore
December 14, 2025 AT 13:48