When cancer spreads, it doesn’t just damage organs-it can throw your body’s chemistry out of balance. One of the most dangerous imbalances is hypercalcemia of malignancy, where calcium levels in the blood spike dangerously high. This isn’t just a lab result. It causes confusion, extreme fatigue, nausea, kidney failure, and even coma. For decades, calcitonin has been one of the fastest tools doctors use to bring those levels down. But it’s not a cure. It’s a bridge-and knowing how and when to use it can make all the difference.
What Happens When Cancer Raises Calcium Levels?
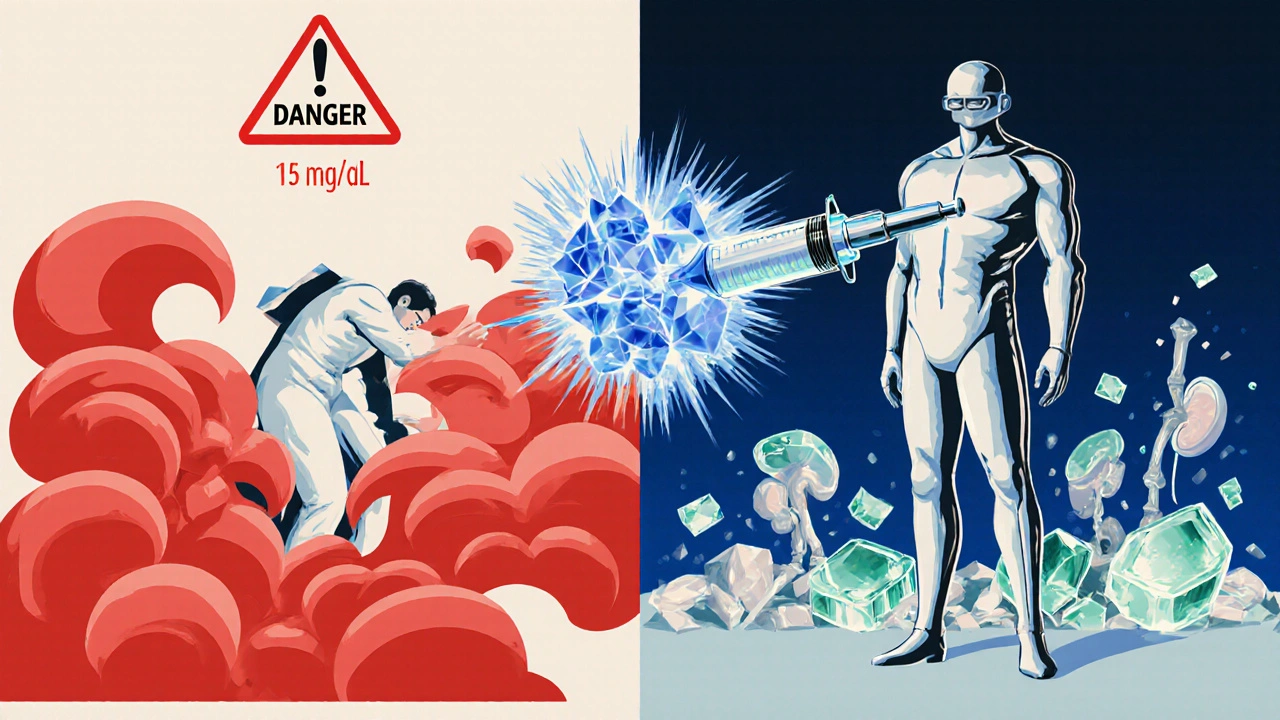
Hypercalcemia of malignancy isn’t caused by eating too much dairy. It’s triggered by tumors that either release substances that trick bones into breaking down (like PTHrP-parathyroid hormone-related protein) or spread into bone tissue and directly destroy it. When bone breaks down, calcium floods into the bloodstream. Levels above 12 mg/dL are dangerous. Above 15 mg/dL? That’s a medical emergency.
Patients don’t just feel tired. They get dehydrated because high calcium makes them pee constantly. Their kidneys struggle. Their nerves misfire. Their heart rhythm can change. In advanced cancer, this isn’t a side effect-it’s a life-threatening complication. And it happens in up to 30% of people with advanced solid tumors, especially breast, lung, and multiple myeloma.
Why Calcitonin? Speed Matters
There are several ways to lower calcium: IV fluids, bisphosphonates, denosumab, dialysis. But none of them act fast. Bisphosphonates take 24 to 48 hours to start working. That’s too long if someone is confused, vomiting, or in heart distress.
Calcitonin is different. It’s a hormone naturally made by the thyroid. It tells bone cells (osteoclasts) to stop breaking down bone. It also tells the kidneys to dump more calcium into urine. The result? Calcium levels can drop by 1 to 2 mg/dL within just 2 to 6 hours after a single injection.
That speed is why calcitonin is still used-especially in hospitals. It’s the go-to drug when you need to stabilize a patient fast while waiting for longer-acting treatments to kick in.
How Is Calcitonin Given?
Calcitonin is given as a shot under the skin or into a muscle. The standard dose is 4 IU per kilogram of body weight, every 12 hours. For an average adult, that’s about 200 IU every 12 hours. It’s usually given for 2 to 5 days, until bisphosphonates or denosumab take over.
It’s not a pill. It’s not an IV drip. It’s an injection. And it’s not cheap. A vial of synthetic calcitonin can cost over $200. That’s why it’s not used long-term. But for a critical 48 hours? The cost is worth it.
What Are the Side Effects?
Calcitonin is generally safe-but it’s not harmless. The most common side effects are nausea and vomiting. About half of patients feel sick after the first dose. Flushing, dizziness, and tingling in the hands are also common. These usually fade after a few doses.
Some people develop allergic reactions. Rarely, there’s a drop in blood pressure. Long-term use can lead to tolerance-meaning the body stops responding. That’s why it’s never used for more than a few days. Also, calcitonin doesn’t work well in patients with kidney failure. If the kidneys can’t flush calcium out, the drug loses its power.
Why Isn’t Calcitonin the First Choice Anymore?
It’s not that calcitonin doesn’t work. It’s that better tools exist now.
Bisphosphonates like zoledronic acid and pamidronate lower calcium more deeply and last longer-up to 4 weeks. Denosumab, a newer antibody, works even better in some cancers, especially multiple myeloma. Both are now the standard first-line treatments.
But here’s the catch: they take days to work. So doctors don’t stop using calcitonin. They use it as a starter. Think of it like putting on a seatbelt while you wait for the car to start. You don’t need it for the whole trip, but you need it right now.
When Do Doctors Still Choose Calcitonin?
There are three clear situations where calcitonin still makes sense:
- Severe, symptomatic hypercalcemia-especially if the patient is confused, vomiting, or has an irregular heartbeat. Time is critical.
- When bisphosphonates can’t be used-like in patients with severe kidney disease who can’t handle IV bisphosphonates.
- As a bridge-while waiting for denosumab to be ordered or delivered, which can take 24-48 hours in some hospitals.
In one 2023 study from the UK’s National Cancer Registry, calcitonin was used in 18% of hypercalcemia cases in advanced cancer patients. In 82% of those cases, it was given within the first 6 hours of admission-and almost always alongside IV fluids and a bisphosphonate.
What About Calcitonin’s Future?
Calcitonin is fading from guidelines as a standalone treatment. The American Society of Clinical Oncology no longer lists it as a primary option. But it hasn’t disappeared. In fact, some hospitals still keep it in their emergency kits.
Why? Because sometimes, speed beats perfection. If a patient is crashing, you don’t wait for the perfect drug. You use what works now. Calcitonin still saves lives in those moments.
There’s also research into synthetic versions with longer half-lives. But none have reached the market yet. For now, calcitonin remains a short-term hero in a long-term battle.
What Should Patients Know?
If you or someone you love has cancer and high calcium, calcitonin might be part of the plan. But it’s not the endgame. It’s the first step. Ask your doctor: “Is this for immediate relief while we start the real treatment?” If the answer is yes, then you’re in the right place.
Don’t be alarmed if you feel sick after the injection. That’s normal. But if you feel faint, your heart races, or you break out in a rash, tell the nurse right away.
And remember: calcitonin won’t cure your cancer. But it can buy you time-time to get stronger, to start the real treatment, to breathe easier.
Key Takeaways
- Calcitonin lowers blood calcium fast-within hours, not days.
- It’s used for severe, symptomatic hypercalcemia of malignancy, not as a long-term fix.
- Side effects include nausea, flushing, and dizziness, but they usually fade.
- Bisphosphonates and denosumab are now first-line treatments, but they take longer to work.
- Calcitonin is still essential in emergencies, kidney failure, or when other drugs aren’t available.
Can calcitonin cure hypercalcemia of malignancy?
No, calcitonin does not cure hypercalcemia of malignancy. It only lowers calcium levels temporarily. The root cause is the cancer itself, and treating the cancer-through chemotherapy, radiation, or targeted therapy-is what ultimately resolves the high calcium. Calcitonin is a supportive treatment used to stabilize patients while longer-term therapies take effect.
How long does calcitonin last in the body?
Calcitonin has a short half-life of about 4 to 6 hours. That’s why it’s given every 12 hours. Its effect on calcium levels usually lasts 12 to 24 hours, which is why repeated doses are needed. After 48 hours, its effect starts to weaken as the body becomes tolerant to it.
Is calcitonin safe for elderly cancer patients?
Yes, calcitonin is generally safe for elderly patients, but it requires careful monitoring. Older adults are more likely to experience nausea and dizziness. They may also have reduced kidney function, which limits how well calcitonin works. Doctors often lower the dose or avoid it entirely if kidney function is poor. In most cases, it’s still used short-term because the risks of untreated high calcium are greater.
Can calcitonin be taken orally?
No, calcitonin cannot be taken orally. Like many hormones, it’s broken down by stomach acid and digestive enzymes. That’s why it must be injected-either under the skin (subcutaneous) or into the muscle (intramuscular). There is no effective oral form available.
Why isn’t calcitonin used more often today?
Calcitonin is used less often because newer drugs like bisphosphonates and denosumab are more effective and longer-lasting. They reduce calcium more deeply and prevent rebounds. Calcitonin’s effects are short-lived, and tolerance develops quickly. It’s now reserved for urgent cases where speed is critical, not for routine management.


Charlos Thompson
October 29, 2025 AT 12:55Oh wow, so calcitonin is the medical equivalent of a Band-Aid on a hemorrhage? Cute. I love how we still cling to this 1970s relic like it’s the last slice of pizza at a party where everyone’s drunk and the fridge is empty. Meanwhile, denosumab’s over there doing backflips while we’re over here injecting hormone soup into grandma’s butt because ‘speed matters.’ Speed? Yeah, speed to get the patient to the ICU before they turn into a human calcium crystal. 🤡
Peter Feldges
October 31, 2025 AT 12:51While the efficacy of calcitonin in acute hypercalcemic crises is well-documented, its utility must be contextualized within the broader therapeutic architecture of oncologic care. The pharmacokinetic profile-namely, its short half-life and propensity for tachyphylaxis-renders it unsuitable for sustained intervention. One must, therefore, regard it not as a definitive modality, but as a temporizing bridge-a physiological pause button-while definitive therapies (e.g., bisphosphonates, denosumab) achieve therapeutic concentration. This is not obsolescence; it is evolution.
Rohit Nair
November 1, 2025 AT 10:01Interesting read. I work in a small hospital in Kerala and we don’t always have denosumab on hand. Calcitonin is our go-to when someone’s calcium hits 16 and they’re barely conscious. It’s not perfect, but it’s something. I’ve seen patients wake up after the first shot-just enough to say ‘thank you’ before the real treatment kicks in. It’s not glamorous, but it’s human.
Wendy Stanford
November 1, 2025 AT 22:19It’s fascinating how medicine clings to the idea of ‘speed’ as a virtue, as if time is the enemy and not the disease itself. We rush to lower calcium because we fear the numbers, not because we understand the person behind the lab result. Calcitonin is a bandage on a soul that’s unraveling-temporary, superficial, emotionally sterile. We treat the ion, not the individual. And in that reductionism, we lose the humanity of care. We are not machines optimizing for lab values-we are witnesses to suffering, and sometimes, the most compassionate thing is to sit with it, not inject our way out of it.
Jessica Glass
November 2, 2025 AT 12:27Oh please. ‘Calcitonin saves lives.’ Right. Like how a sparkler saves a house from burning down. You’re not treating cancer-you’re just making the patient less nauseous while the tumor eats their bones. And let’s not pretend this isn’t just a relic because hospitals are too cheap to stock denosumab properly. If you’re using calcitonin because your pharmacy doesn’t have the real drugs, that’s not ‘clinical wisdom,’ that’s systemic failure dressed up in white coats.
Krishna Kranthi
November 4, 2025 AT 00:57So calcitonin is like that one friend who shows up late to the party but brings the best snacks and makes everyone laugh for 10 minutes before vanishing. Not the main event but damn if you don’t miss them when they’re gone. I’ve seen it in India-doctors use it like a trusty old bike when the ambulance is still 2 hours away. The side effects? Yeah, nausea. But when your mom’s eyes are glassy and she can’t stand up, you’ll take nausea over coma any day. Also, the vial costs more than my monthly phone bill. But hey, at least it works. For now.
Lilly Dillon
November 5, 2025 AT 16:59I read this whole thing. Twice. I didn’t know calcitonin was still used. I thought it was obsolete. I’m glad it’s not. It’s weird how something so old can still be so vital in a moment of crisis. Makes me think about how medicine isn’t about the newest tech-it’s about what works when everything else is too slow.
Shiv Sivaguru
November 6, 2025 AT 06:52Why are we even talking about this? It’s a glorified placebo with side effects. If you’re using calcitonin because you’re too lazy to wait 24 hours for denosumab, you’re doing it wrong. Also, who even stocks this anymore? I’ve never seen it in my hospital. Probably just a relic from the ‘90s that some old doc still clings to like a security blanket. Honestly, if you’re that desperate for speed, just give IV fluids and pray.
Gavin McMurdo
November 7, 2025 AT 21:57Let’s be brutally honest: calcitonin is a glorified Hail Mary. It’s not a treatment-it’s a tactical delay. And yes, it’s still useful. But let’s not romanticize it. The fact that we’re still using a hormone that was discovered in the 1960s because our healthcare system can’t reliably deliver denosumab in under 48 hours is a scandal. Not a triumph. This isn’t ‘speed beats perfection’-this is ‘perfection is too expensive, so we patch the hole with duct tape and hope.’ And if you’re a patient in a rural hospital? You’re the one holding the tape.
Jesse Weinberger
November 8, 2025 AT 06:01Wait wait wait-so calcitonin works for 12 hours and then you need another shot? And it makes you puke? And it’s expensive? And it doesn’t even work if you have kidney issues? So basically it’s like a caffeine pill for cancer? You feel better for a bit, then crash harder? And we’re still using this? I thought we were past this. Did we just forget how to do science? Or are we just addicted to the drama of ‘emergency medicine’? I mean, if you’re this desperate for a quick fix, maybe you shouldn’t be treating cancer at all.