Levofloxacin Tendonitis Risk Calculator
This tool helps assess your personal risk of developing tendonitis while taking levofloxacin. Based on factors mentioned in the article, including age, steroid use, and activity level.
Levofloxacin is a widely prescribed fluoroquinolone antibiotic used for respiratory, urinary and skin infections. While it clears nasty bacteria quickly, it also carries a lesser‑known risk: tendon inflammation and, in rare cases, rupture. Tendonitis refers to inflammation of a tendon, the thick cord that attaches muscle to bone. When an antibiotic like levofloxacin interferes with tendon health, everyday activities can become painful, and athletes may face weeks of rehab.
Why Levofloxacin Affects Tendons
The link starts at the cellular level. Fluoroquinolones bind to bacterial DNA‑gyrase, but they also interact with human collagen‑producing cells called fibroblasts. This interaction can weaken collagen fibers, reduce blood flow, and trigger oxidative stress. Over time, the tendon’s structural integrity declines, making it more vulnerable to micro‑tears that swell into full‑blown tendonitis.
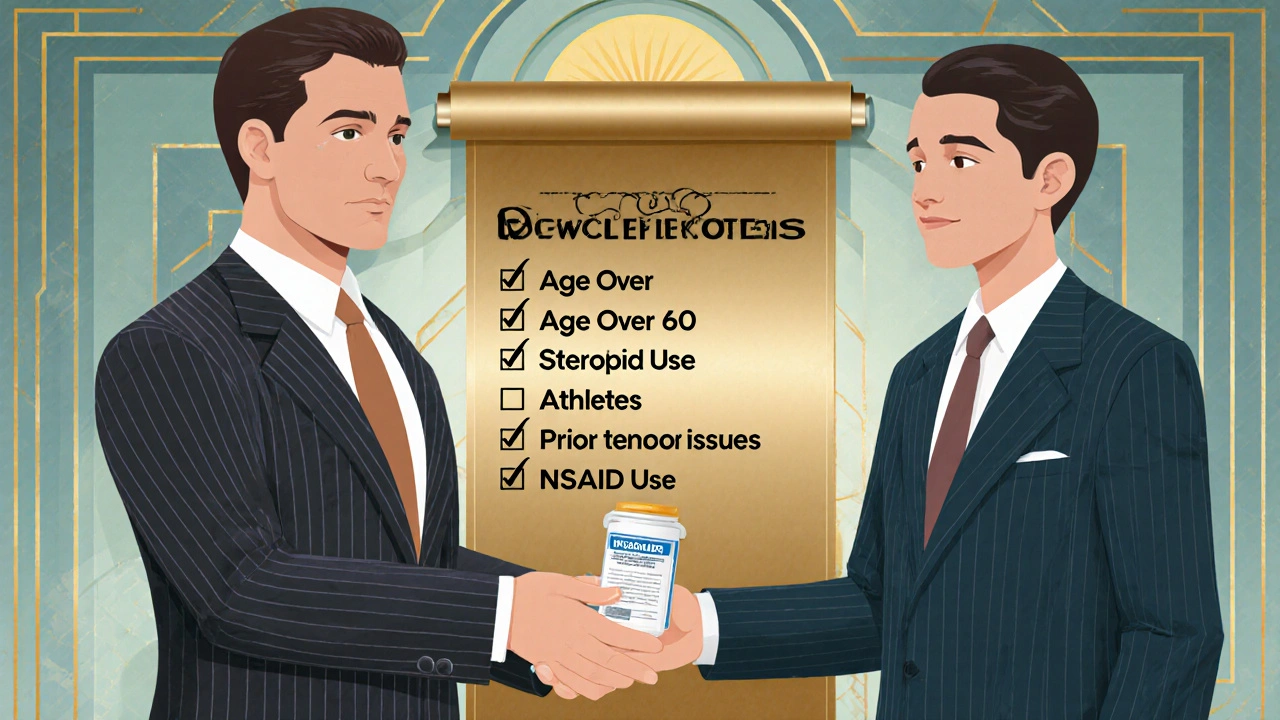
Who Is Most at Risk?
- People over 60 years old - age‑related tendon degeneration amplifies the drug’s impact.
- Patients taking corticosteroids - steroids thin connective tissue, compounding the collagen‑damage risk.
- Athletes or anyone doing high‑impact activities - repetitive stress accelerates tendon wear.
- Individuals with a history of tendon problems - previous injuries lower the threshold for new inflammation.
- Those concurrently using NSAIDs - non‑steroidal anti‑inflammatory drugs can mask early pain, delaying diagnosis.
Understanding these factors helps clinicians decide whether levofloxacin is appropriate or if a safer alternative should be chosen.
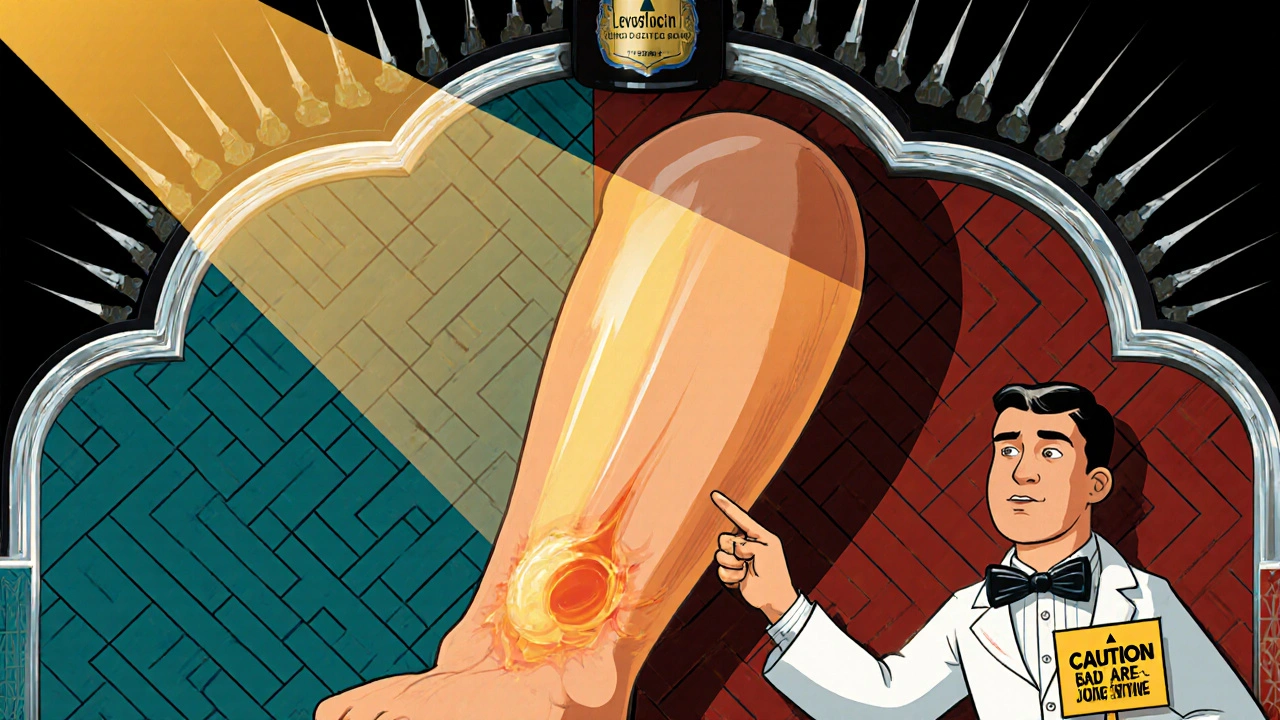
Symptoms to Watch For
Early tendonitis often mimics a muscle strain, but there are tell‑tale signs:
- Sudden, sharp pain near the tendon (commonly the Achilles, rotator cuff, or patellar tendon).
- Swelling or bruising that worsens with movement.
- Limited range of motion - you might notice difficulty climbing stairs or reaching overhead.
- Popping or snapping sensations, especially if a partial tear is forming.
If any of these appear within a few days to weeks after starting levofloxacin, stop the medication (under a doctor’s guidance) and seek medical evaluation.
Comparing Levofloxacin with Other Fluoroquinolones
| Drug | Reported tendonitis incidence (per 10,000 prescriptions) | Typical dosage (mg/day) | Key side‑effects |
|---|---|---|---|
| Levofloxacin | 3.5 | 500-750 | GI upset, QT prolongation |
| Ciprofloxacin | 2.8 | 250-750 | Photosensitivity, CNS effects |
| Moxifloxacin | 1.9 | 400 | Liver enzymes rise, dizziness |
| Ofloxacin | 1.2 | 400 | Rash, tendinopathy (lower rate) |
The numbers come from post‑marketing surveillance data collected by the FDA between 2018 and 2023. While all fluoroquinolones share a tendon‑risk class effect, levofloxacin sits near the higher end of reported cases.
Managing the Risk: What Doctors and Patients Can Do
Prevention is better than rehab. Here’s a practical checklist:
- Screen before prescribing: Ask about age, steroid use, and recent tendon injuries.
- Prefer alternatives (e.g., amoxicillin or doxycycline) when the infection is susceptible.
- Educate patients on early warning signs; give written instructions.
- If therapy must continue, schedule a follow‑up within 7‑10 days to reassess pain.
- Advise patients to avoid high‑impact sports for at least two weeks after finishing the course.
- Encourage adequate hydration - good blood flow supports tendon repair.
When tendonitis does develop, immediate cessation of the drug (with a substitute antibiotic) is the first step. Physical therapy focusing on gentle stretching, followed by gradual strengthening, helps most patients return to normal function within 4-6 weeks.
Legal and Regulatory Outlook
Since the early 2000s, the European Medicines Agency (EMA) and the FDA have required boxed warnings on fluoroquinolone labels. In 2021, the FDA updated its label to emphasize tendon‑rupture risk, especially in patients over 60 and those on steroids. Courts in the United Kingdom have seen several malpractice claims where clinicians failed to warn about tendon risk, leading to increased liability awareness.
Key Takeaways for Everyday Readers
- Levofloxacin can cause tendon inflammation, most often in the Achilles or shoulder area.
- Older adults, steroid users, and athletes are the highest‑risk groups.
- Early symptoms include sharp pain, swelling, and reduced movement - act fast.
- Alternative antibiotics are available for many infections; discuss options with your prescriber.
- If you’re on levofloxacin, stay active but avoid sudden intense workouts until the course ends.
Frequently Asked Questions
Can a single dose of levofloxacin cause tendonitis?
Most tendon issues appear after several days of therapy, but rare cases have been reported after just one dose, especially in people with pre‑existing tendon problems.
Is the risk the same for men and women?
Studies show a slightly higher incidence in women, possibly due to differences in collagen density, but the overall risk pattern (age, steroids) is similar across genders.
What should I do if I develop tendon pain while on levofloxacin?
Stop the medication only after consulting your doctor. They’ll likely switch you to a non‑fluoroquinolone antibiotic and may order imaging (ultrasound or MRI) to assess tendon damage.
Does taking vitamin C reduce the tendon risk?
There’s no solid evidence that vitamin C prevents fluoroquinolone‑related tendonitis. Maintaining a balanced diet is helpful but not a guaranteed protective measure.
Are there any long‑term consequences after tendonitis resolves?
Most patients fully recover with proper rehab. However, a minority experience lingering weakness or scar tissue, raising the chance of future injuries.
Bottom line: Levofloxacin remains an effective weapon against bacterial infections, but it’s not without a tendon‑danger side effect. Knowing who’s at risk, spotting symptoms early, and having a clear plan with your healthcare provider can keep you infection‑free and pain‑free.

Kevin Hylant
October 22, 2025 AT 14:15I’ve seen a lot of people get hit with tendon pain after taking levofloxacin. The risk seems real, especially for older folks. Doctors should flag it before prescribing. If you’re on the drug, watch for sharp pain in the Achilles or shoulder. Stop the med and call your doctor right away.
Craig E
October 31, 2025 AT 19:23Reading through the data, one cannot help but feel a pang of empathy for those caught between infection and injury. It’s a delicate balance: the cure that saves can also sow the seeds of future pain. I appreciate the meticulous table comparing fluoroquinolones – it paints a vivid picture of relative risk. Perhaps the most valuable takeaway is the call for clinicians to practice vigilant prescriptive stewardship. After all, medicine is as much an art of restraint as it is of intervention.
Marrisa Moccasin
November 10, 2025 AT 01:36Did you know!!! The pharma giants are hiding the true extent of tendon damage??? Every time you swallow a pill they’re secretly recording your collagen levels!!!!
Don’t trust the labels – they’re a sham!!
Jonathan Harmeling
November 19, 2025 AT 07:50It’s disheartening to see shortcuts in prescribing, especially when the stakes involve someone’s mobility. While levofloxacin is effective, we must not turn a blind eye to its darker side. People deserve transparent communication, not a shrug and a prescription. If you’re a doctor, ask yourself: am I protecting the patient or just ticking a box? The moral imperative is clear – prioritize safety over convenience.
Ritik Chaurasia
November 28, 2025 AT 14:03In many cultures, the emphasis on holistic health makes us wary of powerful antibiotics like levofloxacin. The tendon risk isn’t just a statistic; it’s a lived reality for athletes and elders alike. We must champion alternatives that respect both the body’s integrity and cultural wisdom. So, let’s push for prescriptions that honor tradition and science together.
Oliver Johnson
December 7, 2025 AT 20:16Honestly, the whole warning thing is overblown. We’re taught to fear every side‑effect, but in the grand scheme levofloxacin still saves lives. If you’re too scared to take it, maybe you’re not cut out for modern medicine. Keep the hype in check and focus on the bigger picture.
Taylor Haven
December 17, 2025 AT 02:30Look, it’s not just about a stray tendon ache after a few days of antibiotics – it’s about a systematic effort to keep the public in the dark about what’s really happening inside their bodies. The pharmaceutical industry has been engineering these fluoroquinolones for decades, knowing full well they can degrade collagen fibers, yet they push them onto the market with a glossy box warning that no layperson truly understands. Meanwhile, regulatory agencies, under pressure from lobbyists, water down the language to something that sounds benign, while the real data – the spikes in Achilles ruptures, the subtle but debilitating chronic tendonitis cases – are buried in endless PDFs that only a handful of diligent researchers ever read. And what about the doctors? They’re bombarded with “quick fix” narratives, where the prescription of a broad‑spectrum antibiotic becomes a reflex rather than a thoughtful decision, especially in an overburdened health system. The result is a cascade of patients, many over 60, who are simultaneously on steroids for inflammation and now a fluoroquinolone that exacerbates the very tissue they’re trying to protect. It’s a perfect storm, engineered and ignored. Add to that the subtle influence of insurance formularies that favor cheaper, high‑volume drugs over safer, perhaps slightly more expensive alternatives, and you see a profit‑driven motive that eclipses patient safety. The very fact that we’re still seeing a higher incidence of tendon injuries with levofloxacin compared to its cousins, as the FDA data plainly shows, is proof that the class effect is being downplayed for commercial convenience. So yes, watch for sharp pain, swelling, limited motion – but also stay vigilant about the larger narrative. Question why the warnings are only now becoming “boxed” after years of neglect, and demand transparency. The risk is real, the mechanisms are understood, and the suffering is avoidable if we choose to challenge the status quo rather than accept it passively.
Sireesh Kumar
December 26, 2025 AT 08:43Alright folks, let me break it down: levofloxacin knocks out the bugs, but it can also mess with your tendons. If you’re over 60 or on steroids, think twice. There are simpler antibiotics that do the job without the tendon drama. So, chat with your doc, ask for alternatives, and keep an eye on any weird aches.
Gary Marks
January 4, 2026 AT 14:56Wow, this article really drags on about the tendon thing, but honestly, who cares? If you’ve got an infection, you need the drug, tendon pain or not. The whole risk talk is just another way to scare people into buying “natural” supplements that don’t work. Let’s be real, the side‑effects are overblown and the doctors know what they’re doing. Stop hyping the drama and trust the prescription.
Vandermolen Willis
January 13, 2026 AT 21:10Thanks for the thorough rundown! 👍 It’s good to know what to watch out for. I’ll keep an eye on any shoulder or ankle pain if I ever need this antibiotic. Stay safe, everyone! 😊
Mary Keenan
January 23, 2026 AT 03:23Skip levofloxacin if you can.