Why Medication Safety Matters More in Kidney Disease
When your kidneys aren’t working right, your body can’t clear drugs the way it should. That means even common medicines can build up to dangerous levels. For someone with chronic kidney disease (CKD), taking the same dose of a pill as a healthy person isn’t just risky-it can be life-threatening. About 1 in 7 adults in the U.S. has CKD, and nearly a third of hospitalizations in this group are tied to medication errors. The problem isn’t always that doctors prescribe wrong doses. Often, it’s that no one checks.
How Kidney Function Changes How Drugs Work
Your kidneys filter waste, including leftover drugs. When kidney function drops, those drugs stick around longer. This isn’t true for all medications, but for many, it’s a big deal. The key number doctors use is eGFR-estimated glomerular filtration rate. It tells you how well your kidneys are filtering blood. A normal eGFR is above 90. Once it drops below 60, most guidelines say you need to rethink your meds.
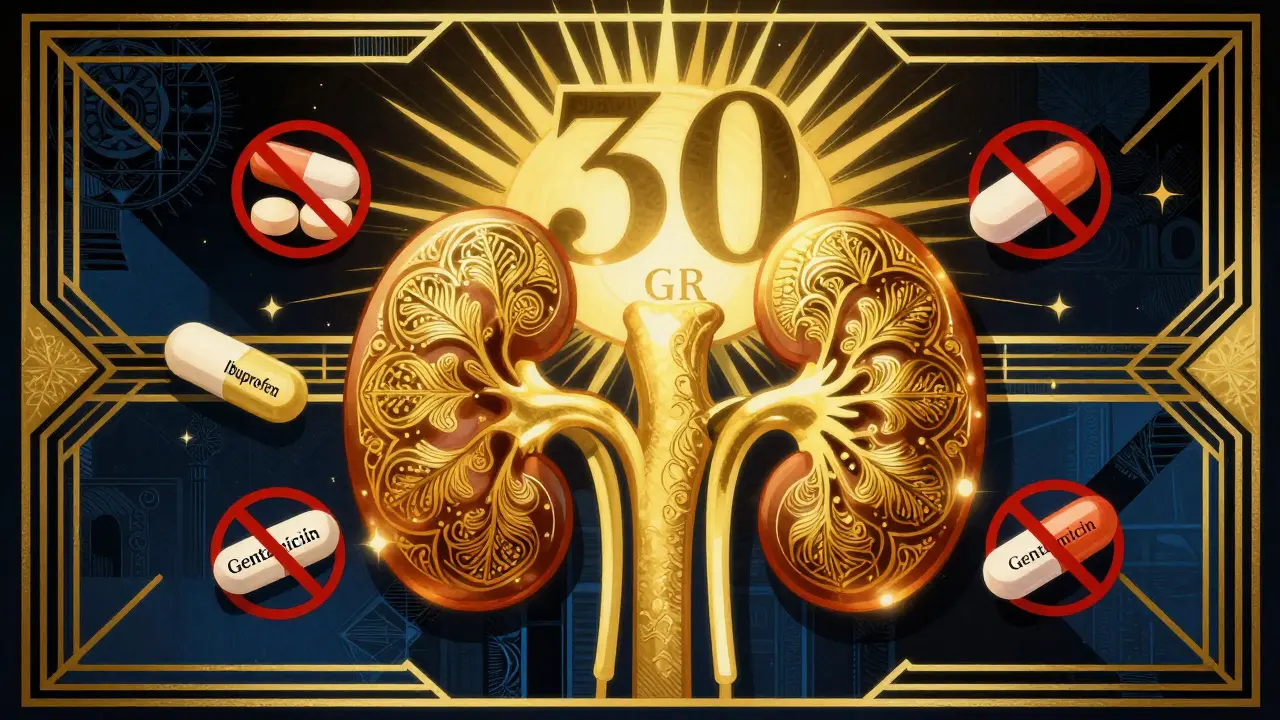
Drugs like gentamicin, vancomycin, and many antibiotics are cleared almost entirely by the kidneys. If your eGFR is 30, you might need to take the same drug only every 48 hours instead of every 8. Miss that adjustment, and you risk hearing loss, nerve damage, or even kidney failure. The same goes for painkillers. NSAIDs like ibuprofen and naproxen can cause sudden kidney injury, even in people with mild CKD. One patient on Reddit described taking two Advil for a headache and ending up in the hospital with his creatinine jumping from 3.2 to 5.7 in under two days.
Which Medications Are Most Dangerous?
Not all drugs are created equal when it comes to kidney safety. Some are outright risky. Others are safe if used correctly. Here’s what to watch for:
- NSAIDs (ibuprofen, naproxen, celecoxib): These reduce blood flow to the kidneys. Even short-term use can trigger acute kidney injury in CKD patients.
- Metformin: A common diabetes drug. It’s safe down to an eGFR of 30. Below that, it’s contraindicated because of lactic acidosis risk. Many patients don’t know this-68% of CKD patients say they’re unsure which over-the-counter or prescription drugs are safe.
- Contrast dye: Used in CT scans. Can cause contrast-induced nephropathy. If you have CKD, ask if a safer alternative exists, or if hydration protocols can be used first.
- Sodium phosphate bowel prep: Used before colonoscopies. Can cause severe kidney damage. Polyethylene glycol (PEG) is the safer choice for CKD patients.
- Some antivirals and antifungals: Like acyclovir or amphotericin B. Require careful dosing or avoidance.

What’s Changed in the Latest Guidelines (2024)
The 2024 KDIGO guidelines brought major shifts in thinking. One of the biggest? Stop holding back on ACE inhibitors and ARBs because your creatinine goes up. For years, doctors worried that rising creatinine meant the drugs were hurting the kidneys. But now we know: that rise is often a sign the drugs are working. These medications protect the kidneys long-term, even when eGFR is below 30. Not using them at full dose is now considered suboptimal care.
Another game-changer: SGLT2 inhibitors like dapagliflozin. Unlike almost every other kidney-related drug, they don’t need dose adjustments-even when eGFR drops below 25. They’ve been shown to cut the risk of kidney failure by nearly 40%. And they’re now recommended even for people without diabetes. That’s huge. These drugs are changing how we treat CKD-not just managing it, but slowing its progress.
Also new in 2024: finerenone. It’s a non-steroidal mineralocorticoid receptor antagonist. If you have albuminuria (protein in your urine) despite being on maximum ACE/ARB therapy, and your potassium is under 4.8, finerenone can add another layer of protection. It’s not for everyone, but for the right patient, it’s a powerful tool.
How to Avoid Dangerous Drug Interactions
It’s not just about single drugs. It’s about combinations. Take a CKD patient on an ACE inhibitor, a diuretic, and an NSAID. That’s a triple threat. The ACE/ARB lowers blood pressure and protects kidneys. The diuretic removes fluid. The NSAID blocks kidney blood flow. Together, they can crash kidney function fast. That’s why medication reviews are critical.
Experts recommend a full drug review every three months for anyone with stage 3 or worse CKD. That means listing every pill, supplement, and OTC medicine. Don’t forget herbal products-some, like St. John’s Wort or licorice root, can interfere with blood pressure meds or raise potassium. A 2022 study found that nearly 24% of CKD patients were on at least one medication that didn’t match their kidney function. Electronic health records often don’t flag these errors. That’s why using one pharmacy for all your prescriptions matters. Pharmacists can catch interactions your doctor might miss.
Practical Steps for Safer Medication Use
If you have kidney disease, here’s what you can do right now:
- Know your eGFR. Ask your doctor for the number and what it means. Don’t just accept “your kidneys are slow.”
- Keep a current list of every medication, including doses and why you take them. Bring it to every appointment.
- Never take NSAIDs without checking. Use acetaminophen (Tylenol) instead for pain, unless your doctor says otherwise.
- Ask about alternatives. For diabetes, is metformin still safe? Could an SGLT2 inhibitor or GLP-1 agonist work better?
- Use a renal dosing app. Tools like Epocrates or Medscape have renal dosing calculators built in. Many nephrologists use them daily.
- Get a medication review. Ask your pharmacist or nephrologist for a full audit at least twice a year.

What Happens When You Don’t Adjust Doses?
The consequences aren’t theoretical. In hospitals, 41% of facilities don’t have protocols for adjusting meds during acute kidney injury. That means a patient with CKD admitted for pneumonia might get a full dose of an antibiotic meant for someone with healthy kidneys. Within days, their kidneys can crash. They might need dialysis. They might never recover full function.
One man in his 60s with stage 4 CKD was prescribed a standard dose of ciprofloxacin for a UTI. His eGFR was 28. He developed severe nausea, confusion, and seizures. His drug levels were dangerously high. He spent two weeks in the hospital. He survived, but his kidney function dropped further. That could’ve been prevented with a simple dose adjustment.
What’s Next for Kidney Medication Safety?
The future is moving toward smarter systems. The FDA is planning a 2026 update to its guidance, using real-world data from electronic records to refine dosing rules. The KDIGO group is developing a standardized checklist for CKD patients before surgery or imaging-something every clinic should use. And research is underway to see if genetic testing can predict how someone’s body will handle certain drugs based on their kidney function.
For now, the best protection is awareness. Know your numbers. Ask questions. Don’t assume a prescription is safe just because it’s been taken for years. Kidney disease doesn’t care about your age, your insurance, or how long you’ve been on a drug. It only cares about function-and what you’re putting into your body.
Key Takeaways
- Always check your eGFR before starting or changing any medication.
- NSAIDs and contrast dye are high-risk-avoid them unless absolutely necessary.
- Metformin is unsafe below eGFR 30; SGLT2 inhibitors are safe across all stages.
- ACE inhibitors and ARBs should be used at full dose, even if creatinine rises.
- Use one pharmacy and get a full medication review every 3-6 months.