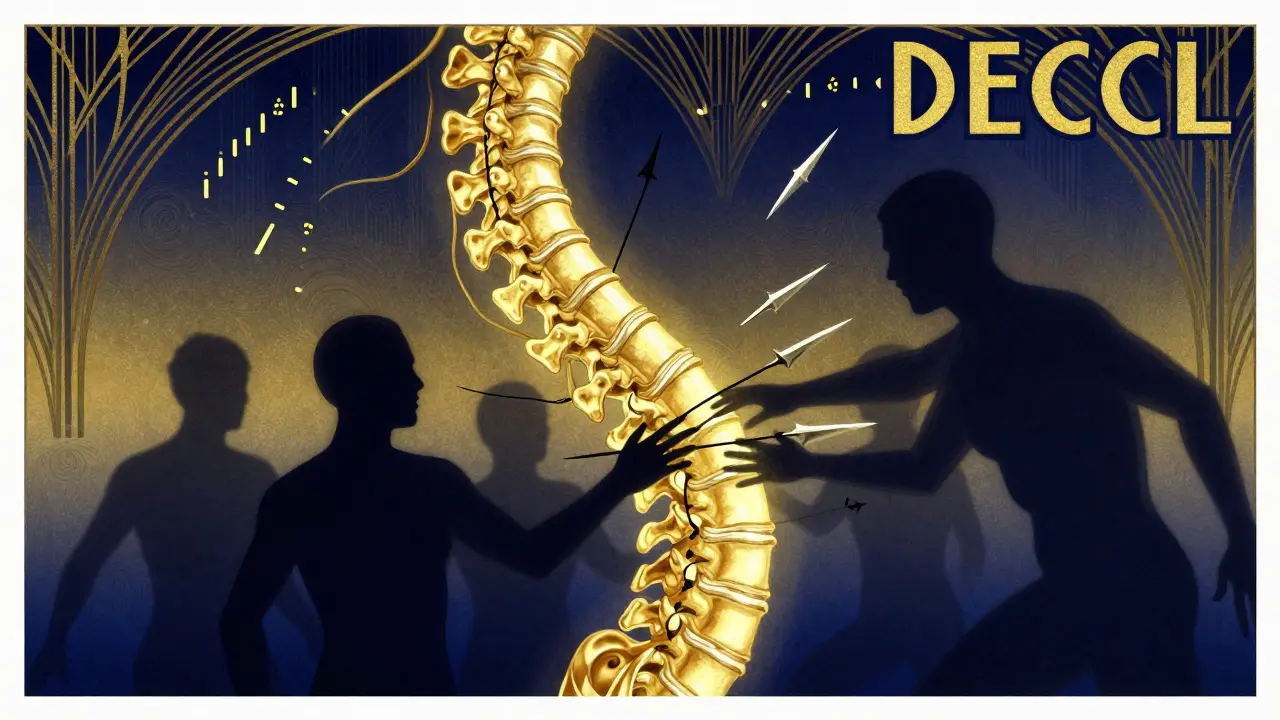
What Really Happens in Multiple Sclerosis?
Multiple Sclerosis isn’t just about flare-ups and fatigue. At its core, it’s a slow, silent war inside your brain and spinal cord. Your immune system, which should protect you, starts attacking the protective coating around your nerves - the myelin sheath. This isn’t a one-time event. It keeps happening, over and over. Each attack leaves behind damage. And while some of that damage can heal, especially early on, the real problem isn’t the inflammation - it’s what happens after.
When myelin is stripped away, the nerve fibers underneath - called axons - start to suffer. At first, they might just slow down. Signals from your brain to your legs, or your hands, get fuzzy. You might feel numbness, tingling, or weakness. But if the myelin doesn’t come back, the axon itself begins to break down. And once an axon dies, it doesn’t grow back. That’s why so many people with MS slowly lose function over time, even when their flare-ups stop.
Why Some People Get Worse Even When They’re Not Flaring Up
Most people with MS start with relapsing-remitting MS (RRMS). That means they have clear attacks - maybe vision problems, leg weakness, or loss of balance - followed by periods where things get better, sometimes almost completely. About 85% of people are diagnosed this way. But here’s the catch: after 10 to 15 years, about 40% of them shift into a different phase called secondary progressive MS (SPMS). In this stage, symptoms keep getting worse, even if there are no new flare-ups. No new lesions on MRI. No spikes in inflammation. Just steady decline.
What’s driving that? It’s not the same immune attack anymore. The inflammation moves from the bloodstream into the brain and spinal cord itself. Immune cells, especially B cells, gather in the meninges - the membranes around the brain - and form structures that look like tiny lymph nodes. These become factories for ongoing damage. They release chemicals that slowly poison nerve cells. Meanwhile, the axons that lost their myelin years ago are running on empty. They’re missing mitochondria - the power plants of the cell. They’re losing sodium channels that keep signals moving. They’re degenerating, not from an outside attack, but from internal failure.
Why Current Treatments Don’t Stop Progression
Right now, there are 21 FDA-approved drugs for MS. They’re called disease-modifying therapies (DMTs). And they’re good at one thing: reducing relapses. In RRMS, these drugs can cut flare-ups by 30% to 50%. That’s huge. They stop new lesions from forming on MRI. They delay disability for years. But they don’t fix what’s already broken. And they barely touch the damage happening in SPMS or primary progressive MS (PPMS).
Why? Because DMTs target inflammation. They calm the immune system. They block immune cells from crossing into the CNS. But once the disease shifts from inflammation-driven to degeneration-driven, those drugs lose their power. You can’t stop axons from dying by turning down the immune system. You need to protect the axons themselves. That’s the missing piece.

What’s Really Causing the Permanent Damage?
It’s not just the loss of myelin. It’s what happens to the axon after. Studies using advanced MRI show that even areas of the brain that look normal on a regular scan - called normal-appearing white matter - are already damaged. Magnetization transfer ratio (MTR) drops, signaling loss of tissue structure. Post-mortem exams reveal axons with fragmented neurofilaments, missing mitochondria, and swollen, dysfunctional axoplasm. The nerve fibers aren’t just bare - they’re starving.
One major theory is that without myelin, axons have to work harder. Myelin normally lets signals jump quickly from one node to the next. Without it, the axon has to fire continuously along its whole length. That burns through energy. And over time, the axon runs out of fuel. Mitochondria can’t keep up. Sodium pumps fail. The axon starts to swell, then break. This is why disability keeps climbing even when inflammation fades.
Another key player? Astrocytes. These are support cells in the brain. In MS, they lose a specific receptor - the β2-adrenergic receptor. That receptor normally helps them respond to norepinephrine, a chemical that keeps brain cells healthy. When it’s gone, astrocytes can’t protect neurons properly. They might even start contributing to damage. This isn’t just about immune cells attacking. It’s about the brain’s own support system breaking down.
What’s on the Horizon? New Treatments Beyond Inflammation
Scientists aren’t waiting. There are 17 active clinical trials right now targeting progressive MS. These aren’t just more immune suppressants. They’re trying to do things like:
- Protect mitochondria - giving nerve cells the energy they need to survive
- Block sodium channels - so axons don’t overwork and burn out
- Stimulate remyelination - helping the body regrow myelin
- Block regeneration inhibitors - like Nogo, MAG, and LINGO-1, proteins that stop nerves from repairing themselves
One promising area is drugs that target the Nogo receptor. In animal studies, blocking this pathway allowed damaged nerves to regrow. Human trials are underway. Another is Siponimod, already approved for SPMS, which doesn’t just calm inflammation - it may directly protect nerve cells.
But the biggest breakthrough might come from measuring damage differently. MRI scans showing brain shrinkage - especially in gray matter - are now better predictors of future disability than the number of lesions. The Multiple Sclerosis Functional Composite (MSFC) test, which measures walking speed, hand dexterity, and thinking, is becoming more important than the old EDSS scale. That’s because it catches the real problem: the brain’s ability to function.

What This Means for You Right Now
If you have RRMS, starting a DMT early isn’t optional - it’s critical. The sooner you reduce inflammation, the less axonal damage you’ll accumulate over time. It’s like stopping a leak before the floor rots. Even if you feel fine, the damage is happening under the surface.
If you’re in SPMS and still having flare-ups, some DMTs may still help. But if you’re past that stage, your focus needs to shift. Exercise matters - not just for strength, but for brain health. Aerobic activity boosts blood flow and may help protect neurons. Physical therapy keeps muscles active and prevents secondary complications. Diet and vitamin D aren’t cures, but low levels are linked to worse outcomes. Don’t smoke. Smoking doubles your risk of progression.
And stay informed. The next five years will bring real change. Treatments that protect nerves, not just calm the immune system, are coming. The goal isn’t just to stop relapses anymore. It’s to stop the slow fade.
Why Axon Loss Changes Everything
For decades, MS was seen as a disease of myelin. Now we know better. Myelin damage causes the flare-ups. But axon loss causes the permanent disability. That’s why someone can have a great MRI - no new lesions - and still be losing the ability to walk. The damage isn’t visible on standard scans. It’s happening at the level of the nerve fiber itself.
This shift in understanding explains why some people respond to treatment and others don’t. It explains why progressive MS feels so hopeless. And it’s why the future of MS care isn’t just about more drugs - it’s about smarter ones. Drugs that don’t just fight inflammation, but rebuild what’s been lost.

wendy parrales fong
December 25, 2025 AT 17:56It’s wild how we’ve been treating MS like it’s just an immune glitch, when really it’s more like a house with a busted foundation. You can patch the roof all you want, but if the beams are rotting, the whole thing’s gonna collapse. I never realized axons could just... starve. That’s haunting.
And the part about astrocytes losing their receptor? That’s like losing your best friend who used to remind you to eat and sleep. Now they’re just standing there, useless. Makes you wonder what else in the brain is quietly giving up.
Jeanette Jeffrey
December 27, 2025 AT 13:05Oh please. Another ‘MS is secretly degeneration’ sob story. You think we didn’t know axons die? The whole field’s been chasing myelin like it’s the Holy Grail because pharma doesn’t want to fund hard science. They’d rather sell you a pill that ‘reduces relapses’ than admit we have zero tools to fix broken neurons. Wake up. This isn’t a revelation-it’s a 20-year-old paper with a new PowerPoint.
carissa projo
December 27, 2025 AT 17:53Jeanette, I hear you-and I get the frustration. But dismissing this as ‘old news’ ignores the real shift: we’re finally seeing the *mechanism*, not just the symptom. It’s like realizing your car won’t start not because of the battery, but because the fuel lines are clogged with rust. You can keep jumping it, sure. But until you clean the lines? It’s just a band-aid.
And that’s why the new trials? They’re not just ‘more drugs.’ They’re trying to *rebuild*. To nourish. To give axons back their mitochondria, their sodium channels, their dignity. That’s not hype. That’s hope with a lab coat.
david jackson
December 28, 2025 AT 04:03Okay, so imagine your nervous system is a highway system, right? Myelin is the asphalt-smooth, fast, efficient. When it’s gone, the axons are like cars trying to drive on gravel with no suspension, no gas, and the engine’s on fire. And the worst part? The traffic cops-the immune system-are still pulling over people for speeding, while the whole road is crumbling underneath them. And now we’re learning that the road crew isn’t even showing up anymore. The astrocytes? They’re the ones who used to fix potholes and refill the gas stations… and now they’ve quit. And nobody told them they were supposed to be the heroes. This isn’t just science. It’s a tragedy written in neurons.
And yet-we’re not giving up. We’re looking at drugs that don’t just shut down the cops, but rebuild the damn road. That’s not just progress. That’s a miracle in the making.
Jody Kennedy
December 29, 2025 AT 13:58I’ve been on Tecfidera for 7 years. Still walking. Still working. Still laughing. If you told me 10 years ago I’d be this stable, I’d have called you a liar. DMTs aren’t perfect-but they’re the reason I’m still here. Don’t let the ‘progressive MS’ doom talk erase that. I’m proof that early action works.
And yeah, I’m scared of what’s coming next. But I’m also excited. Because if we’re finally looking at axons like living things that need care-not just targets to avoid-then maybe we’re on the edge of something real.
christian ebongue
December 29, 2025 AT 15:07DMTs work for RRMS. That’s it. Stop pretending they’re magic. SPMS? You’re on your own. Go walk. Take D. Don’t smoke. That’s your ‘treatment.’ The rest is marketing.
Also, ‘Nogo receptor’? Sounds like a rejected Marvel villain.
Alex Ragen
December 30, 2025 AT 04:21One must, however, critically interrogate the epistemological foundations of this narrative: is the axonal degeneration model truly *causal*, or merely correlative? Are we conflating biomarkers-MTR, gray matter atrophy-with pathogenesis? And what of the confounding variables: vascular insufficiency, mitochondrial polymorphisms, gut-brain axis dysregulation? The reductionist framing of ‘myelin bad, axons sad’ is dangerously simplistic-almost… populist. One must ask: who funds these trials? Who profits from the ‘neuroprotection’ buzzword? The answer, I suspect, lies not in the cerebellum-but in the balance sheets.
Still. The science is fascinating. Even if it’s all a distraction.
Lori Anne Franklin
December 30, 2025 AT 21:17My dad has PPMS. He can’t walk anymore. But he still reads me poetry every night. I don’t know if science will fix him-but I know love hasn’t left yet. Keep fighting, everyone. Even if the meds don’t work, your heart still does.