When you fill a prescription for a drug like warfarin, levothyroxine, or lithium, you might assume the pharmacist can swap the brand name for a cheaper generic without issue. But in many states, that’s not allowed-no matter how much money you save. The truth is, NTI substitution laws vary wildly across the U.S., creating a confusing patchwork of rules that can affect your health, your wallet, and your daily routine.
What Exactly Is an NTI Drug?
NTI stands for Narrow Therapeutic Index. These are medications where even tiny changes in dosage can lead to serious harm-or even death. Think of it like walking a tightrope: one step too far, and you fall. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid issues), and certain anti-seizure medicines fall into this category. A 5% difference in absorption might mean your blood doesn’t clot properly, or your seizures return. The FDA says all approved generics are just as safe and effective as brand names. But many states don’t trust that.Why Do States Have Their Own Rules?
Even though the FDA doesn’t officially label drugs as NTI, state pharmacy boards started creating their own lists back in the mid-1990s. Why? Because patients and doctors reported problems after switching from brand to generic. A patient on warfarin might have a dangerous spike in INR levels. Someone on levothyroxine might feel exhausted, gain weight, or develop heart issues. These weren’t just theories-they were real cases. So states stepped in to protect people, even if it meant going against federal guidance.Three Main Types of NTI Substitution Laws
States handle NTI drugs in one of three ways:- Carve-outs: These states ban substitution entirely for certain NTI drugs. Kentucky, for example, has a formal list of 27 drugs-including digoxin, lithium, and all strengths of levothyroxine-that pharmacists cannot substitute without explicit written permission from the doctor.
- Affirmative consent: In states like North Carolina and Connecticut, both the doctor and the patient must sign off before a generic can be given. In Connecticut, if you’re on an anti-seizure drug, the pharmacist must notify your doctor and you within 72 hours of substitution. If either objects within 14 days, the switch is canceled.
- Notification-only: Some states, like South Carolina, don’t ban substitution but require pharmacists to document it and inform the prescriber. It’s advisory, not mandatory.
Which States Are the Strictest?
Kentucky leads the pack with the most detailed and restrictive rules. Their list isn’t just broad categories-it’s specific drug strengths. For example, levothyroxine 0.05 mg is on the list, but 0.025 mg isn’t. That level of detail forces pharmacists to check every prescription manually. In North Carolina, you need two signatures: one from your doctor and one from you. In Pennsylvania, substitution is outright prohibited for any drug on their official NTI list.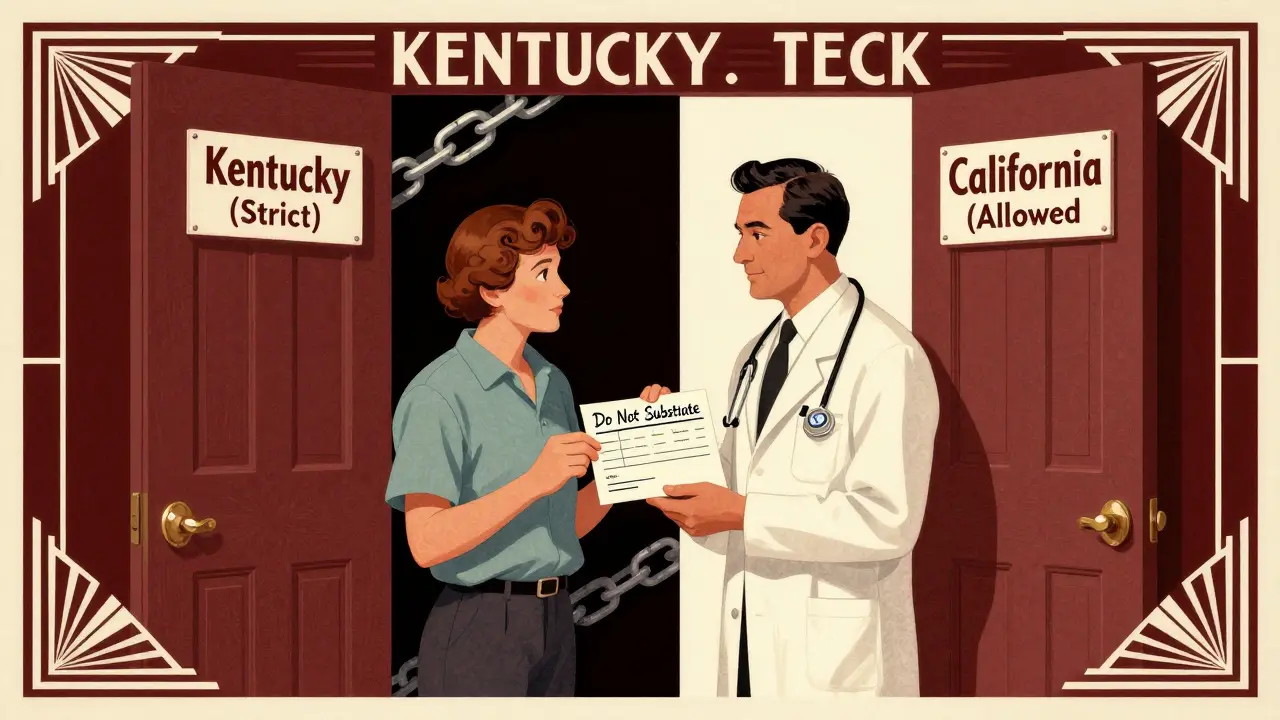
Which States Don’t Care?
On the other end, states like California, Texas, and Virginia follow the FDA’s lead. If a generic is approved as therapeutically equivalent, it can be swapped without extra steps. Pharmacists in these states report fewer delays, lower administrative costs, and patient complaints under 0.5%. A 2022 study found that in states without NTI restrictions, generic use for these drugs was 12.4% higher than in states with strict rules.The Real Cost of These Laws
These rules aren’t just about safety-they’re about money. NTI drugs cost over $28 billion a year in the U.S. When states block substitution, patients pay more. A single pill of brand-name Synthroid can cost $50. The generic? $10. In Kentucky, you’re likely paying the higher price unless your doctor writes “Do Not Substitute” on the prescription. That adds up fast for people on lifelong meds. Pharmacists also pay a price. In states with strict rules, it takes an average of 3.2 minutes to verify if a drug can be substituted. In states without rules? Less than a minute. That’s over 8 extra hours a month just for compliance. Many pharmacies now use software that auto-checks state lists, but small, independent pharmacies still struggle.What’s Changing?
There’s growing pressure to fix this mess. In 2023, California passed a law requiring NTI designations to be based on scientific evidence-not tradition. New York and Ohio are now reviewing their lists using the FDA’s new draft guidance, which suggests a drug should only be labeled NTI if the ratio between toxic and effective dose is 2.0 or lower. That could remove dozens of drugs from state lists that don’t truly belong there. The Association for Accessible Medicines is even suing Kentucky, arguing their rules create an unfair barrier to interstate commerce. If courts side with them, it could force states to align more closely with federal standards.
What Should You Do?
If you take an NTI drug:- Know your state’s rules. Check your state pharmacy board’s website.
- Ask your pharmacist: “Is this drug on the NTI substitution list here?”
- If you’re switched without consent, speak up. You have rights.
- Keep a list of your NTI meds and the exact brand or generic you’re on. Don’t assume the next refill will be the same.
Is This Really Necessary?
The debate isn’t settled. The FDA says there’s no proof generics are less safe. Studies show no difference in INR control between brand and generic warfarin in over 12,000 patients. But hospital pharmacists? 78% still believe certain NTI drugs need special handling. And for patients who’ve had bad experiences-like uncontrolled seizures or dangerous bleeding-it’s not about data. It’s about trust.What’s Next?
The National Association of Boards of Pharmacy is working on a model NTI framework to bring some consistency to the chaos. It’s expected in late 2023. But with 27 states already having their own rules, change won’t come fast. For now, if you’re on a critical medication, don’t assume anything. Ask questions. Know your rights. And keep track of what’s in your bottle.Are all generic NTI drugs unsafe?
No. The FDA approves all generics for NTI drugs based on strict bioequivalence standards. Most patients switch without any issues. But because these drugs have very little room for error, even small differences in how the body absorbs them can matter for some people. That’s why some states require extra steps-not because generics are unsafe, but because the consequences of a bad switch can be severe.
Can I request a brand-name NTI drug even if my state allows substitution?
Yes. In every state, you have the right to ask for the brand-name version. Your pharmacist must honor that request, even if substitution is allowed. You may pay more, but you control your treatment. Always tell your pharmacist if you’ve had problems with a generic in the past.
Which NTI drugs are most commonly restricted?
The most common NTI drugs on state lists are warfarin (blood thinner), levothyroxine (thyroid hormone), lithium (mood stabilizer), phenytoin and carbamazepine (anti-seizure), and digoxin (heart medication). These are the ones most likely to be blocked from substitution, regardless of your state.
Does my doctor need to know if I’m switched to a generic?
In states with affirmative consent or notification laws, yes-your doctor must be informed. Even in states without rules, it’s a good idea to tell your doctor if your generic was switched. They may want to check your blood levels, especially for drugs like warfarin or lithium.
Why do some states include drugs that aren’t truly NTI?
Many state lists were created decades ago based on anecdotal reports or outdated studies. Some drugs on the lists, like Premarin or Synthroid, aren’t classified as NTI by modern standards. But once a law is passed, it’s hard to remove drugs without a formal review. Newer laws, like California’s, are starting to fix this by requiring scientific evidence before adding a drug to the list.


Robin Keith
January 29, 2026 AT 10:53Look, I get it-pharmacists are just trying to save a buck, but when your life hangs on a 5% variance in absorption, you don’t want some algorithm deciding what’s ‘therapeutically equivalent’… The FDA doesn’t live in your body, and no spreadsheet can measure the tremor in your hands after a switch. I’ve seen it: my uncle’s INR went from 2.3 to 4.8 after they swapped his warfarin-no warning, no consent, just a different pill in the bottle. He nearly bled out in his sleep. And now? They call it ‘bioequivalence.’ Funny how the word ‘equivalent’ sounds so clean when you’re not the one gasping for air in the ER…