More than 1 in 5 adults in the UK reach for an over-the-counter sleep aid at least once a month. You’re not alone if you’ve tried Benadryl, Unisom, or a melatonin gummy after a bad night. But here’s the truth most labels won’t tell you: these products aren’t magic pills. They’re temporary fixes with real risks - especially if you use them too long.
How OTC Sleep Aids Actually Work
Most OTC sleep aids fall into two camps: antihistamines and supplements. Antihistamines like diphenhydramine (in Nytol, Sominex) and doxylamine (in Unisom SleepTabs) were never meant to help you sleep. They were designed to treat allergies. The drowsiness? That’s just a side effect. These drugs block histamine, a brain chemical that keeps you alert. Less histamine = sleepiness. Simple.
Melatonin is different. It’s a hormone your body naturally makes at night to signal it’s time to rest. Supplements try to mimic that signal. But here’s the catch: a 2017 study found that melatonin products on shelves often contain way more - or way less - than what’s on the label. One bottle might have 83% less than advertised. Another might have nearly five times as much. You’re guessing what you’re taking.
Valerian root and chamomile? They’re herbal. No strong evidence they work better than a placebo for most people. But they’re low-risk, so many try them anyway.
The Real Side Effects You Can’t Ignore
Antihistamine-based sleep aids don’t just make you sleepy. They can leave you foggy, dry-mouthed, and confused the next day. One in three users report dry mouth. One in five say their vision blurs. For men over 50 with prostate issues, these drugs can make it hard to urinate. For older adults, the risks are worse.
A 2015 study tracking over 3,400 people for more than seven years found that long-term use of antihistamines like diphenhydramine was linked to a 54% higher risk of dementia. That’s not a small number. It’s a red flag. The American Geriatrics Society now says these drugs should be avoided in people over 65. Why? Because they increase fall risk by half. One stumble can mean a broken hip - and a lifetime of pain.
Melatonin sounds safer, but it’s not harmless. Nearly half of users report daytime drowsiness. Almost 7 in 10 say they have wild, vivid dreams - or nightmares. Higher doses (over 5mg) raise the risk of nausea, dizziness, and even bedwetting in kids. The NHS warns that melatonin can cause leg pain. If it doesn’t go away in a few days, stop taking it.
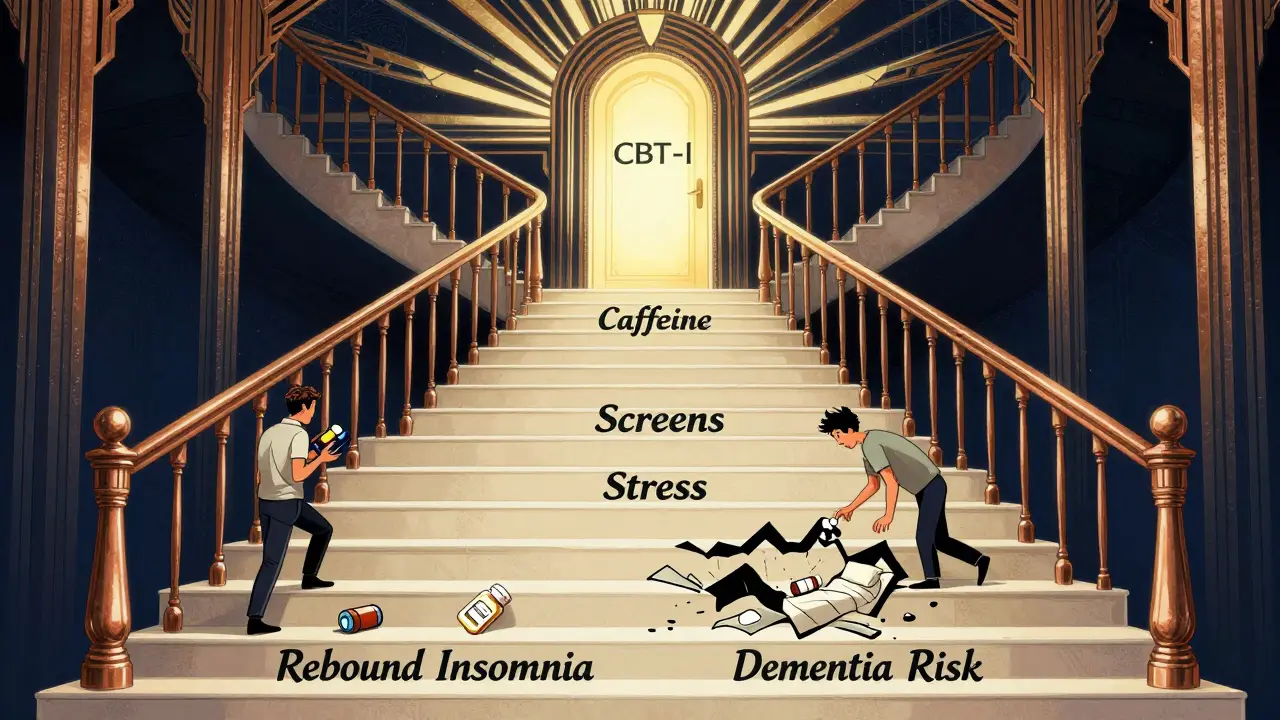
And then there’s rebound insomnia. If you use these aids for more than two weeks, your body starts to rely on them. When you stop, sleep gets worse than before. About 30% of long-term users experience this. You think you’re helping yourself. You’re training your brain to need a pill to sleep.
Who Should Avoid OTC Sleep Aids Completely
Not everyone should touch these products. If you have sleep apnea, OTC sleep aids can be dangerous. They relax your throat muscles, making breathing interruptions worse. That’s not a risk you want to take.
Pregnant women should avoid them too. Diphenhydramine is labeled as Category B - no proven harm, but not enough data to say it’s safe. Melatonin? Even less is known. The NIH says there’s no reliable safety data for use during pregnancy.
And if you’re over 65? The Beers Criteria - the gold standard for safe prescribing in older adults - lists diphenhydramine and doxylamine as potentially inappropriate. That means the risks outweigh any tiny benefit. The NHS, Harvard, and the American Academy of Sleep Medicine all agree: skip them.

What the Labels Don’t Say About Safe Use
Every box says: “Do not use for more than two weeks.” But a 2022 survey found nearly 4 in 10 people use them longer. Some for months. Why? Because they think it’s harmless. It’s not.
For antihistamines, the FDA’s limit is clear: two weeks max. After that, talk to a doctor. For melatonin, the European Food Safety Authority says 1mg is enough for most adults. Anything higher doesn’t help - it just adds side effects. Yet most bottles sell 3mg, 5mg, or even 10mg. You’re overdosing by default.
Start low. Try 0.5mg of melatonin. One pill. One night. See what happens. Don’t take it every night. Use it only for jet lag or a rare bad night. Daily use leads to tolerance. One study found 25% of people who took OTC sleep aids every day for 10 days stopped responding to them.
What Actually Works Better - and Lasts Longer
The best treatment for insomnia isn’t a pill. It’s CBT-I - Cognitive Behavioral Therapy for Insomnia. It’s not magic. It’s work. But it works. Studies show 70-80% of people who complete CBT-I see lasting improvement. That’s better than any medication.
CBT-I teaches you how to fix your sleep habits. It helps you stop lying in bed awake, trains your brain to associate your bed with sleep, and reduces the anxiety that keeps you up. No pills. No side effects. No rebound.
Other simple fixes? Cut caffeine after 2pm. Get sunlight in the morning. Keep your bedroom cool and dark. No screens an hour before bed. These aren’t just tips. They’re science-backed tools. And they work for people who’ve tried everything else.
When to Call a Doctor
If you’ve been struggling with sleep for more than three weeks, it’s not just stress. It’s insomnia. And it needs real help.
Don’t wait until you’re taking melatonin every night and still waking up at 3am. Don’t wait until you’re dizzy in the morning or forgetting names. See your GP. Ask about CBT-I. Ask about sleep studies. There are options that don’t come in a bottle.
OTC sleep aids might feel like a quick fix. But they’re a trap. They give you a little sleep now - and steal your natural rhythm later. Your body knows how to sleep. You just need to help it, not drug it.
Final Thought: Sleep Is Not a Problem to Be Fixed
You don’t need a pill to sleep. You need rest. You need routine. You need peace. OTC sleep aids might help for one or two nights - maybe if you’re jet-lagged or recovering from a bad day. But they’re not a solution. They’re a distraction from the real work: rebuilding your sleep habits.
If you’re tired of relying on pills, you’re not broken. You’re just human. And humans were never meant to need a chemical to rest. Start small. Be patient. Your body will thank you.
Are OTC sleep aids safe for long-term use?
No. Antihistamine-based sleep aids like diphenhydramine and doxylamine are not safe for long-term use. They’re linked to increased dementia risk, falls in older adults, and rebound insomnia. Melatonin is safer short-term but can cause next-day drowsiness and vivid dreams. Medical guidelines recommend using these products for no more than 7-10 days, and never longer than two weeks without seeing a doctor.
Can melatonin help with jet lag?
Yes, melatonin can help with jet lag, especially when crossing three or more time zones. The best approach is to take 0.5mg to 1mg about 30 minutes before your target bedtime in the new time zone. Start the night you arrive. Don’t take it every day - just for a few nights until your body adjusts. Higher doses (over 5mg) don’t help more and can cause side effects like headaches or nausea.
Why do I feel groggy after taking OTC sleep aids?
Antihistamines like diphenhydramine don’t just help you fall asleep - they linger in your system. Their effects can last 6-8 hours, sometimes longer, especially in older adults. This causes next-day drowsiness, poor focus, and slowed reaction times. About 42% of users report moderate to severe grogginess. Melatonin can cause similar effects if taken too late or in too high a dose.
Is it safe to take OTC sleep aids with alcohol?
No. Mixing alcohol with antihistamine-based sleep aids can dangerously increase drowsiness, slow your breathing, and raise your risk of falls or accidents. Alcohol also disrupts sleep quality, making the problem worse. Even if you’ve had one drink, avoid taking diphenhydramine or doxylamine. The combination is not worth the risk.
What are the best non-drug ways to improve sleep?
The most effective non-drug method is CBT-I (Cognitive Behavioral Therapy for Insomnia), which has a 70-80% success rate. Simple daily habits also help: get morning sunlight, avoid screens before bed, keep your bedroom cool and dark, and go to bed only when sleepy. Avoid caffeine after 2pm. Stick to a consistent wake-up time - even on weekends. These changes rebuild your natural sleep rhythm without side effects.
Can OTC sleep aids cause addiction?
OTC sleep aids aren’t addictive in the same way as prescription sedatives, but they can lead to psychological dependence. Many people feel they can’t sleep without them after using them for more than two weeks. Stopping can trigger rebound insomnia - where sleep gets worse than before. This creates a cycle where you keep using them just to feel normal. That’s not addiction, but it’s still a problem that needs to be broken.

Poppy Newman
January 8, 2026 AT 09:01Sai Ganesh
January 9, 2026 AT 06:18steve rumsford
January 9, 2026 AT 09:48Andrew N
January 10, 2026 AT 22:56Christine Joy Chicano
January 11, 2026 AT 08:40Adam Gainski
January 11, 2026 AT 09:46Anastasia Novak
January 12, 2026 AT 02:29Katrina Morris
January 13, 2026 AT 14:36Ayodeji Williams
January 13, 2026 AT 16:57Kamlesh Chauhan
January 14, 2026 AT 17:02Elen Pihlap
January 15, 2026 AT 21:57Alex Danner
January 17, 2026 AT 08:51LALITA KUDIYA
January 18, 2026 AT 23:55Paul Mason
January 19, 2026 AT 02:22Anthony Capunong
January 20, 2026 AT 16:52