Most people think ear infections only happen inside the ear-like the kind kids get after a cold. But there’s another kind that hits hard after a swim, a shower, or even a humid day: otitis externa, or swimmer’s ear. It doesn’t come from water trapped in the middle ear. It starts in the outer canal-the narrow tunnel between your ear opening and your eardrum. When that skin gets irritated, wet too long, or scratched, bacteria or fungi move in. And it hurts. Not just a little ache. A deep, throbbing pain that makes chewing, talking, or even lying on your pillow unbearable.
Why Your Ear Hurts After Swimming
Swimmer’s ear isn’t just about water. It’s about what happens when your ear’s natural defenses break down. Your ear canal has a built-in shield: earwax. It’s not dirt. It’s a protective layer that keeps moisture out and keeps the pH slightly acidic-around 5.0 to 5.7. That acidity stops most germs from growing. But when you swim often, use cotton swabs, or wear hearing aids or earbuds for hours, you wipe away that shield. Water stays trapped. The skin swells. And suddenly, your ear canal is a perfect breeding ground.The main culprits? Pseudomonas aeruginosa, a bacteria common in pools and hot tubs, and Staphylococcus aureus, which lives on your skin. Together, they cause about 70% of cases. Fungi like Aspergillus show up in 1 in 10 cases, especially if you’ve used antibiotics before or live in a damp climate. The CDC estimates 1 in 10 Americans gets swimmer’s ear each year. Kids between 7 and 12 are most at risk-probably because they swim more and their ear canals are smaller. But adults 45 to 64 aren’t safe either, especially if they have diabetes, which slows healing and raises infection risk.
How Bad Is It? Mild, Moderate, or Severe
Not all swimmer’s ear is the same. It comes in three levels, and knowing which one you have tells you exactly what to do.- Mild: Your ear itches. Maybe a little redness. Slight discomfort when you tug your earlobe. This is the easiest to fix. About 45% of cases fall here.
- Moderate: The canal starts to swell. You feel fullness. Hearing gets muffled. Pain gets sharper, especially when you move your jaw. This happens in 35% of cases.
- Severe: The canal is completely blocked by swelling. Pain is intense. You might have a fever over 101°F, swollen lymph nodes, or even drainage. This is rare-only 20% of cases-but dangerous. Left untreated, it can spread to the bone behind the ear (malignant otitis externa), which is life-threatening.
Most people don’t realize how quickly it can escalate. What starts as an itch can turn into a 48-hour nightmare if you ignore it or try to clean it with a Q-tip. The worst thing you can do is stick anything into the canal. You’re not cleaning it-you’re pushing debris deeper and scraping the skin, making it worse.
The Best Ear Drops for Swimmer’s Ear
Treatment isn’t one-size-fits-all. The right drop depends on what’s causing the infection and how bad it is.For mild cases: Over-the-counter 2% acetic acid with hydrocortisone (like Swim-Ear or VoSoL HC Otic) works wonders. It’s cheap-around $15-and kills bacteria while calming inflammation. Studies show it clears up mild infections in 85% of cases. It’s also great for prevention. If you swim often, put a few drops in after you get out. It lowers your chance of getting infected by 65%.
For moderate to severe cases: You need prescription drops. The gold standard is ciprofloxacin 0.3% with dexamethasone 0.1% (Ciprodex). It’s a combo of a powerful antibiotic and a steroid. The antibiotic kills the bugs. The steroid reduces swelling so the medicine can reach the infection. FDA trials show 92% of people are healed in 7 days. It’s not cheap-$147.50 without insurance-but it works fast. Many users report pain dropping by 80% in under 24 hours.
Another option is ofloxacin (generic Ciprodex). It’s slightly less effective but costs about $45. If you can’t afford Ciprodex, this is your best bet. Avoid older drops like neomycin-polymyxin. They’re cheaper, but they carry a risk of permanent hearing damage if your eardrum is perforated-even if you don’t know it is. The FDA warns against them for this reason.
For fungal infections: If your ear itches like crazy, has white or black debris, and doesn’t improve with antibiotic drops, you likely have a fungus. Clotrimazole 1% solution is the go-to. It’s not available OTC in the U.S., so you need a prescription. Studies show it clears up fungal ear infections in 93% of cases. Acetic acid won’t touch it.

Why Debridement Is the Secret Weapon
Here’s what most people miss: drops alone won’t fix a blocked ear canal. If there’s pus, wax, or dead skin clogging the tunnel, the medicine can’t reach the infection. That’s where debridement comes in.This isn’t something you do at home. A doctor uses a suction device or tiny tools under a magnifying scope to gently clean out the canal. It’s quick. It’s not fun, but it’s not painful. And it makes the drops work 30-40% better. The NIH and Mayo Clinic both say this step is critical. Yet, 60% of patients skip it because they don’t know to ask for it. If you’ve been using drops for two days and nothing’s changed, go back. Ask for your ear to be cleaned.
How to Use Ear Drops Correctly
Even the best drops fail if you use them wrong. Here’s how to do it right:- Wash your hands.
- Warm the bottle in your hands for 1-2 minutes. Cold drops can make you dizzy.
- Lie on your side with the infected ear facing up.
- Pull your earlobe gently up and back (for adults) or down and back (for kids) to straighten the canal.
- Put in the exact number of drops prescribed.
- Stay still for 5 minutes. Don’t sit up. Don’t shake your head. Let the medicine soak in.
- Wipe away any excess with a clean cloth. Never stick cotton into the canal.
Most people skip step 5. They think, “I put the drops in, I’m done.” But if you sit up right away, half the medicine just drains out. That’s why 32% of users report poor results-they’re not letting the drops sit.
What Doesn’t Work (And What Could Make It Worse)
Stop doing these things:- Cotton swabs: They push wax and bacteria deeper. They’re the #1 cause of swimmer’s ear.
- Home remedies like vinegar and alcohol: Vinegar alone won’t kill all bacteria. Alcohol dries out the skin and makes it more prone to cracking. It’s not a substitute for medical treatment.
- Oral antibiotics: The American Academy of Otolaryngology says they add almost nothing to treatment. They increase side effects like diarrhea or yeast infections without improving outcomes.
- Waiting it out: If it’s not better in 48 hours, see a doctor. Delaying treatment raises your risk of complications.
Also, don’t assume your ear pain is swimmer’s ear. Earaches can be from a cold, a tooth infection, or even TMJ. If you have fever, dizziness, or facial weakness, get checked immediately. Those aren’t signs of simple swimmer’s ear.
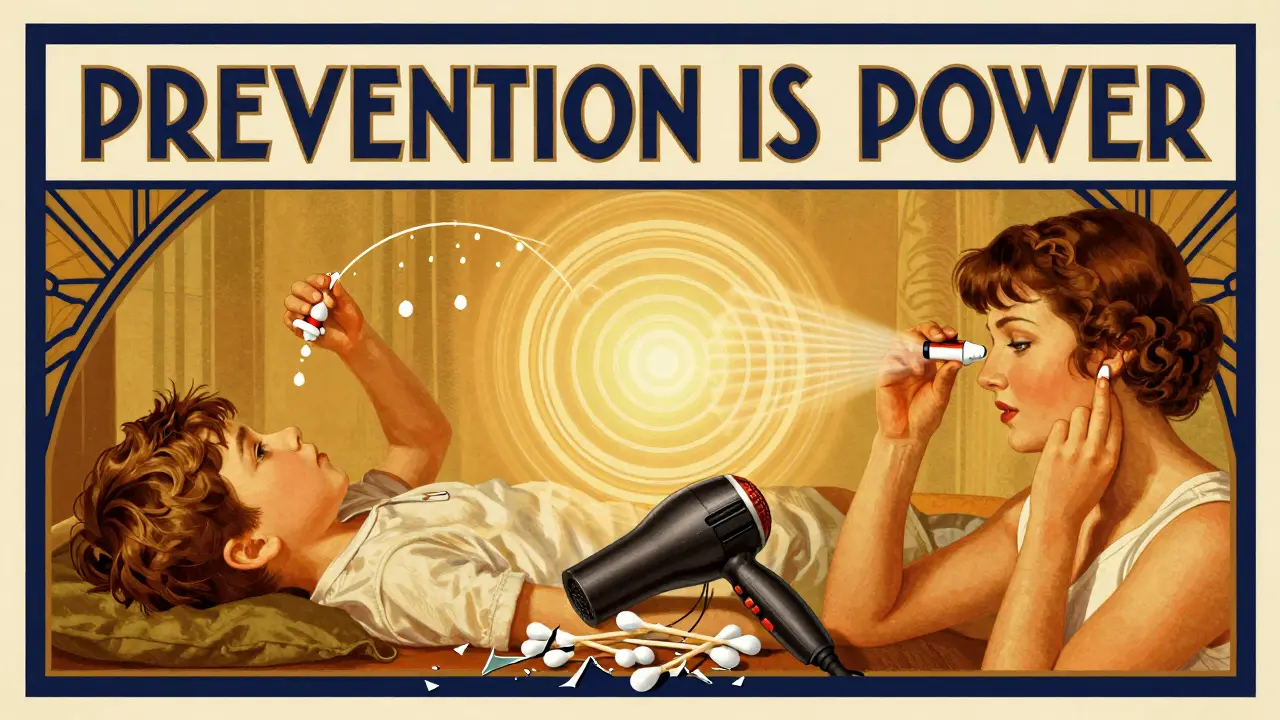
Prevention: How to Keep It From Coming Back
If you swim often, prevention is easier than treatment. Here’s what works:- Use 2% acetic acid drops after swimming or showering. Just 3-4 drops per ear. Let them sit for a minute, then tilt your head.
- Wear a swim cap or silicone earplugs designed for swimming. Regular earplugs can trap water if they don’t fit right.
- Dry your ears with a hairdryer on low, from a distance. Hold it 12 inches away and move it gently.
- Never use cotton swabs, bobby pins, or fingers to clean inside your ear.
- If you have diabetes, check your ears regularly. Even mild irritation can turn serious fast.
People who use drops after swimming reduce their risk by two-thirds. That’s not magic. That’s science.
What’s New in Treatment
In March 2023, the FDA approved a new version of ofloxacin called OtiRx. It’s designed to last 24 hours instead of 12, so you only need one dose a day. Early results show 94% success. It’s not widely available yet, but it’s coming.Researchers at Stanford are also testing treatments that restore the ear’s natural microbiome-like probiotics for your ear. It’s still in trials, but the idea is simple: instead of killing all bacteria, help the good ones come back. That could mean fewer infections long-term.
For now, the best treatment is still the old-school approach: clean, medicate, and prevent. But now you know which drops work, how to use them, and what to avoid.
Can swimmer’s ear go away on its own?
Mild cases might improve in a few days without treatment, but it’s risky. Pain can worsen, swelling can block the canal, and bacteria can spread. Most doctors recommend starting treatment right away. Waiting increases the chance of needing stronger medication or even a procedure to clean the ear.
Are ear drops safe for children?
Yes, but only the right ones. Ciprofloxacin-dexamethasone drops are approved for kids over 6 months. Avoid aminoglycoside drops like neomycin in children unless a doctor confirms the eardrum is intact. Always use the dose your doctor prescribes. Never use adult drops on a child without checking.
Why does my ear sting when I use the drops?
Stinging is common, especially with acetic acid or if the skin is raw. It usually lasts 10-20 seconds. If the burning lasts longer than a minute, or if you get swelling or a rash, stop using it. You might be allergic to a component. Talk to your doctor about switching to a different formula.
Can I use leftover ear drops from last time?
No. Once opened, most ear drops expire in 30 days. Even if they look fine, they can grow bacteria. Using old drops could make your infection worse. Always get a fresh prescription or buy a new OTC bottle.
Do I need to see a doctor for swimmer’s ear?
If your pain is mild and you’ve had it before, you can try OTC drops first. But if you have swelling, fever, hearing loss, or no improvement in 48 hours, see a doctor. If you have diabetes, a weakened immune system, or a history of ear surgery, see a doctor immediately. Self-treatment can delay proper care and lead to serious complications.


Danielle Stewart
December 18, 2025 AT 20:59I used to think swimmer’s ear was just a myth until I got it after a beach trip last summer. The pain was unreal-like someone was stabbing my ear with a hot needle every time I talked. I tried vinegar and alcohol like some Reddit post suggested. Big mistake. Burned like hell and made it worse. Then I went to the doc, got Ciprodex, and within 12 hours the pain dropped like a rock. Don’t mess around. Just get the right drops.
Also, debridement? Total game changer. I didn’t even know it was a thing until my ENT did it. Felt like a tiny vacuum cleaner in my ear. Weird, but holy crap it helped. I wish I’d known this six months ago.
Glen Arreglo
December 20, 2025 AT 19:09For real, the acetic acid drops after swimming are the only reason I haven’t had swimmer’s ear since I started competitive swimming in college. I’ve been doing it for 12 years now. Three drops, wait a minute, tilt. Done. No drama. No pain. No doctor visits. It’s not magic, it’s just basic hygiene. Why do people wait until they’re in agony to start caring?
Also, never use cotton swabs. Ever. Your ear is not a vacuum cleaner filter. Stop trying to clean it. It cleans itself.
shivam seo
December 21, 2025 AT 15:12Lmao another ‘medical expert’ post. You act like you’re the first person to discover that water in ears causes infections. Newsflash: this has been known since the 1950s. And you’re selling Ciprodex like it’s a miracle drug. It’s just a combo of generic antibiotics. The real issue? Big Pharma pushing expensive prescriptions when OTC stuff works fine for 80% of cases.
Also, ‘debridement’? Sounds fancy. It’s just a doctor scraping your ear with a hook. I’ve seen it. It’s unnecessary 90% of the time. Stop fearmongering. People don’t need to panic every time they get wet.
benchidelle rivera
December 23, 2025 AT 12:35As a nurse who’s treated dozens of swimmer’s ear cases in urgent care, I can confirm: 90% of patients come in because they used Q-tips. It’s heartbreaking. You wouldn’t stick a toothbrush into your throat, but you’ll jam a cotton swab into your ear canal like it’s a vacuum?
And yes, Ciprodex works. But if you’re diabetic or immunocompromised, don’t wait. I had a 62-year-old patient last month who delayed treatment because he ‘thought it’d go away.’ He ended up with malignant otitis externa. Required six weeks of IV antibiotics. Don’t be that guy. Your ear is not a DIY project.
Matt Davies
December 24, 2025 AT 03:53Man, I used to be the guy who’d swim every day and then scrub his ears like he was polishing a car. Then I got swimmer’s ear so bad I couldn’t sleep for three nights. I thought I was tough. Turns out I was just dumb.
Now I use those acetic acid drops religiously. Like brushing my teeth. I even keep a tiny bottle in my swim bag. It’s not glamorous, but it’s the only reason I still swim without fear. And I swear, the moment I feel that weird tickle? Drops. No questions. No waiting. Just action.
Also, the hairdryer trick? Genius. Low heat, arm’s length, gentle motion. Feels like a spa for your ear. Do it after every shower too. Your future self will thank you.
Alana Koerts
December 24, 2025 AT 17:16pascal pantel
December 25, 2025 AT 09:56Let’s cut through the noise. The CDC data is misleading. Swimmer’s ear incidence is inflated because primary care docs overdiagnose it to justify prescriptions. Most mild cases are just seborrheic dermatitis or eczema of the canal. You’re being sold a narrative to push Ciprodex. That $147 bottle? It’s not worth it unless you’re immunocompromised.
And debridement? It’s a revenue generator. Most ENTs do it because they get reimbursed for it, not because it’s clinically essential. The NIH says it’s ‘critical’? That’s a guideline, not a law. Use acetic acid. Wait 72 hours. If it doesn’t improve, then go in. Don’t let fear drive your healthcare decisions.
Gloria Parraz
December 27, 2025 AT 01:46I had swimmer’s ear three times in one year. Three. Times. I thought I was cursed. Then I found out I was using my old ear drops from last season. I didn’t even realize they expired. That’s when I learned: once opened, they’re trash after 30 days.
Now I write the opening date on the bottle with a Sharpie. I also started using silicone swim plugs. Not the cheap foam ones-the custom-fit ones. They cost $60 but last 5 years. Total game changer. I haven’t had it since. And yes, I still swim every day. I just don’t be dumb about it anymore.
Also, warm the drops. Cold ones feel like liquid nitrogen in your ear. It’s not just a tip-it’s a survival tactic.
Sahil jassy
December 28, 2025 AT 14:18Kathryn Featherstone
December 29, 2025 AT 03:19I’m a 58-year-old who’s had swimmer’s ear twice since my hip replacement and diabetes diagnosis. I didn’t realize how dangerous it could be until I read this. The part about malignant otitis externa scared me straight. I’ve started using the acetic acid drops religiously. I even set a reminder on my phone: ‘Post-swim drops.’
Also, I stopped using my earbuds for workouts. I didn’t realize they were trapping moisture. Now I use over-ear headphones. Small change. Huge difference.
Thank you for this. I feel like I finally understand what’s going on in my ear instead of just hoping it goes away.
Nicole Rutherford
December 30, 2025 AT 20:22Chris Clark
January 1, 2026 AT 04:00Just had this last month. I thought I was fine with the OTC stuff, but after 3 days no change. Went in, doc did the suction thing-felt like a tiny robot in my ear-and said, ‘You’ve got a whole lotta gunk in here.’ Turns out I had a fungal infection. Clotrimazole fixed it in 4 days.
Biggest takeaway? Don’t assume it’s bacterial. If it itches like crazy and looks like mold, it’s fungus. And yeah, the drops gotta sit. I used to just lie there for 30 seconds. Now I set a timer. Five minutes. No excuses.
Also, never reuse drops. I did it once. Got it back worse. Lesson learned. Don’t be me.