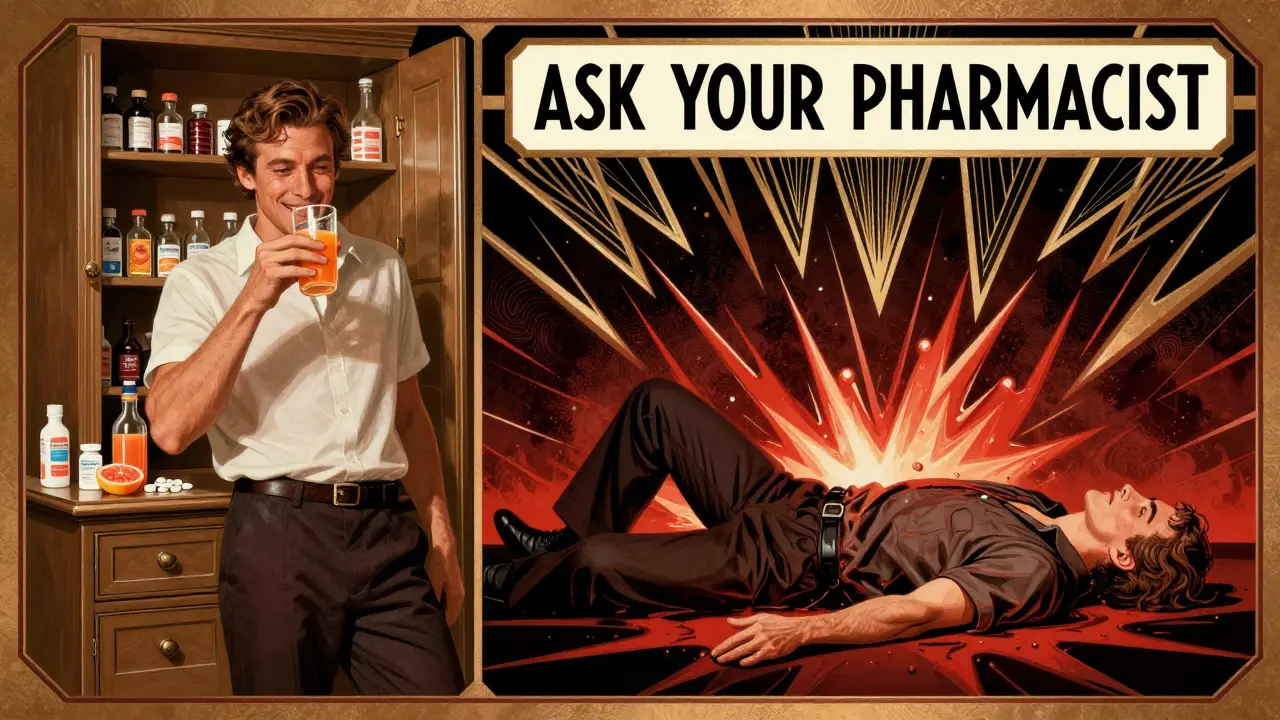
Every year, over a million people in the U.S. end up in the emergency room because of unexpected reactions between their medications. Many of these cases are avoidable. The problem isn’t always the drugs themselves-it’s not knowing how they work together. That’s where your pharmacist comes in. They’re not just the person handing out pills. They’re trained to spot hidden risks in your medicine cabinet that even your doctor might miss.
What Exactly Is a Drug Interaction?
A drug interaction happens when one thing changes how another thing works in your body. It could be another medication, a food, a supplement, or even an existing health condition. These aren’t rare accidents. They’re common-and often silent. You might not feel anything until it’s too late.There are three main types:
- Drug-drug interactions: Two or more medicines react. For example, taking ibuprofen with blood thinners like warfarin can increase your risk of bleeding.
- Drug-food/beverage interactions: Grapefruit juice can make cholesterol or blood pressure meds too strong. Alcohol can make sedatives dangerous. Even high-sodium foods can interfere with heart meds.
- Drug-condition interactions: If you have high blood pressure, decongestants in cold medicines can spike it dangerously. If you have kidney disease, some painkillers can worsen it.
The FDA requires all prescription labels to list known interactions in the “Warnings” section. But that’s just the start. Many interactions-especially with supplements or foods-aren’t always on the label.
What to Ask Your Pharmacist
You don’t need to be a medical expert to protect yourself. Just ask the right questions. Here’s what you should say every time you pick up a new prescription-or even refill one.1. Can this interact with anything else I’m taking?
Don’t just list your prescription drugs. Include everything: over-the-counter painkillers, sleep aids, antacids, allergy meds, and especially supplements. Many people think “natural” means safe. It doesn’t. St. John’s wort can make birth control, antidepressants, and even heart meds stop working. Garlic pills can thin your blood. Turmeric can interfere with diabetes drugs.
Pharmacists see this daily. A 2023 study found that 77% of American adults take at least one supplement. Nearly half of them don’t tell their doctor-or pharmacist. That’s a blind spot you can fix.
2. Should I avoid certain foods or drinks?
Some interactions are simple to avoid-if you know about them.
- Grapefruit juice: Stops your body from breaking down certain statins, blood pressure meds, and anti-anxiety drugs. One glass can make the drug 3 to 5 times stronger.
- Dairy products: Calcium in milk and yogurt can block absorption of antibiotics like ciprofloxacin and tetracycline. Take them 2 hours before or after dairy.
- Alcohol: Combines dangerously with opioids, benzodiazepines, sleep aids, and even some antidepressants. It can cause dizziness, breathing problems, or liver damage.
- High-tyramine foods: If you’re on an MAO inhibitor like phenelzine (Nardil), avoid aged cheeses, cured meats, soy sauce, and tap beer. These can trigger a life-threatening spike in blood pressure.
Ask your pharmacist: “Is there anything in my fridge or pantry I should watch out for?”
3. How will this affect my existing health conditions?
Medications don’t act the same in everyone. A drug that’s fine for one person could be risky for another.
For example:
- If you have heart failure, some NSAIDs (like ibuprofen) can make fluid retention worse.
- If you have diabetes, steroid medications can raise your blood sugar-even if you’re not diabetic.
- If you have kidney disease, many common painkillers and antibiotics need dose adjustments.
Pharmacists check your full medical history. But they can only help if you tell them. Say: “I have [condition]. Will this make it harder to manage?”
4. When and how should I take this?
Timing matters more than you think.
- Some meds work best on an empty stomach-others need food to be absorbed properly.
- Taking two drugs at the same time can cause them to compete for absorption. One might not work.
- Some drugs need to be spaced out by hours. For example, thyroid medicine should be taken alone, at least 30-60 minutes before other meds or food.
Always ask: “Should I take this with food? Should I wait between doses? Is there a best time of day?”
5. What side effects mean I should call you or my doctor?
Not all side effects are serious. But some are red flags.
Ask for a short list of warning signs. For example:
- Unexplained bruising or bleeding (could mean blood thinners are too strong)
- Severe dizziness or fainting (could mean blood pressure dropped too low)
- Swelling in ankles or sudden weight gain (could mean fluid buildup from heart meds)
- Dark urine or yellow skin (could mean liver stress)
Knowing what’s normal versus dangerous gives you control. Don’t wait until you’re in panic mode.
How to Prepare for Your Visit
Pharmacists can’t help if they don’t have the full picture. Bring this with you:
- A written list of all medications: prescriptions, OTC drugs, supplements, vitamins, herbal remedies.
- Each drug’s name, dose, and how often you take it.
- Any recent changes: new meds, stopped meds, changed doses.
- Your usual diet: Do you drink grapefruit juice daily? Eat a lot of leafy greens? Drink alcohol regularly?
- Your medical conditions: diabetes, high blood pressure, kidney issues, liver problems, allergies.
Use your phone’s notes app or a simple piece of paper. Don’t rely on memory. Studies show patients forget or misremember up to half their meds.
Why This Matters More Than Ever
People are taking more medications than ever. Nearly half of adults over 65 take five or more daily. Even younger adults-especially those with chronic conditions-are on multiple drugs.
And it’s not just pills. Supplements are booming. The Council for Responsible Nutrition says 77% of U.S. adults take at least one. Many are unaware these can interact. A 2022 study found that over 18% of dangerous interactions were missed by electronic systems because patients didn’t report their supplements.
Pharmacists are your last line of defense. A 2023 study in the Journal of the American Pharmacists Association showed that when pharmacists did full medication reviews, drug interaction incidents dropped by nearly 24% in Medicare patients.

Don’t Wait for a Problem
You don’t need to wait until you feel sick to talk to your pharmacist. Schedule a quick check-in every three months-or anytime you start, stop, or change a medication. That’s the best way to catch problems before they start.
It’s not about being paranoid. It’s about being informed. Medications save lives. But they can also hurt you if you don’t understand how they work together. Your pharmacist isn’t just there to fill prescriptions. They’re there to keep you safe.
Ask the questions. Bring the list. Speak up. It could be the simplest thing you do to protect your health.
Can over-the-counter medicines interact with prescriptions?
Yes, absolutely. Common OTC drugs like ibuprofen, naproxen, antacids, cold medicines, and sleep aids can interfere with prescriptions. For example, ibuprofen can reduce the effectiveness of blood pressure meds and increase bleeding risk if you’re on warfarin. Antacids with aluminum or magnesium can block absorption of antibiotics like ciprofloxacin. Always check with your pharmacist before taking anything new-even if it’s sold without a prescription.
Do herbal supplements really cause drug interactions?
Yes, and they’re often underestimated. St. John’s wort can make birth control, antidepressants, and HIV meds stop working. Garlic, ginkgo, and ginseng can thin your blood and increase bleeding risk when taken with warfarin or aspirin. Turmeric can lower blood sugar too much if you’re on diabetes medication. Just because something is “natural” doesn’t mean it’s safe to mix with prescription drugs.
Is grapefruit juice really that dangerous with meds?
For some medications, yes. Grapefruit juice blocks an enzyme in your gut that breaks down certain drugs. This can cause the drug to build up to toxic levels. It affects statins (like simvastatin), blood pressure meds (like amlodipine), anti-anxiety drugs (like buspirone), and some immunosuppressants. Even one glass can have effects lasting over 24 hours. If you’re on one of these meds, avoid grapefruit juice entirely. Your pharmacist can tell you if yours is on the list.
Can alcohol interact with my medications?
Definitely. Alcohol can make sedatives, painkillers, antidepressants, and sleep aids much stronger, increasing drowsiness, dizziness, and risk of falls or breathing problems. It can also damage your liver when combined with acetaminophen or certain antibiotics. Even moderate drinking can interfere with diabetes meds, causing dangerous blood sugar swings. Always ask if it’s safe to drink while taking your meds.
How often should I review my medications with a pharmacist?
At least every three months-or anytime you start, stop, or change a medication. Your risk of interactions increases with each new drug. Studies show the most recent medication added is often the one causing the problem. Regular reviews help catch issues early. Many pharmacies offer free medication reviews; ask if yours does.
What if my pharmacist says there’s no interaction, but I still feel weird?
Trust your body. Pharmacists rely on known interactions, but some reactions are rare or individual. If you notice new symptoms-like unusual fatigue, dizziness, nausea, or changes in heart rate-write them down and bring them back. Sometimes it’s a new interaction that hasn’t been widely documented yet. Your feedback helps improve care for others too.
Do pharmacies check for interactions automatically?
Most major pharmacies use electronic systems that flag known interactions. But they only see what you tell them. If you don’t mention a supplement, herbal product, or OTC drug, the system won’t catch it. Studies show these systems miss about 18% of serious interactions because patient histories are incomplete. That’s why your input matters.
Can my diet affect how my medication works?
Yes. Vitamin K in leafy greens like spinach and kale can reduce the effect of warfarin, making your blood clot more easily. High-sodium foods can worsen fluid retention if you’re on heart meds. Dairy can block absorption of some antibiotics. Even caffeine can interfere with asthma or psychiatric medications. Your pharmacist can help you understand how your eating habits connect to your meds.
Next Steps: Take Action Today
Don’t wait for a problem to happen. Grab a pen and write down every medication and supplement you take right now. Include dosages and how often you take them. Bring it to your next pharmacy visit. Ask the five key questions. If you’re unsure, ask for a medication review. It takes 10 minutes-but it could save you a hospital visit.
Medications are powerful tools. But they’re not harmless. The more you know, the safer you are. Your pharmacist is there to help. Use them.


Dylan Smith
December 16, 2025 AT 00:26Ron Williams
December 16, 2025 AT 07:28Aditya Kumar
December 18, 2025 AT 01:51Tiffany Machelski
December 18, 2025 AT 08:22SHAMSHEER SHAIKH
December 20, 2025 AT 06:52Souhardya Paul
December 20, 2025 AT 17:31Josias Ariel Mahlangu
December 22, 2025 AT 02:26anthony epps
December 22, 2025 AT 13:20Andrew Sychev
December 24, 2025 AT 12:03Dan Padgett
December 24, 2025 AT 12:06Hadi Santoso
December 26, 2025 AT 11:36Kayleigh Campbell
December 26, 2025 AT 23:59Joanna Ebizie
December 28, 2025 AT 09:19Elizabeth Bauman
December 30, 2025 AT 03:43Mike Smith
December 30, 2025 AT 17:47