Why sarcopenia in COPD is more dangerous than you think
If you or someone you know has COPD, the biggest threat might not be the coughing or the shortness of breath. It’s the slow, silent loss of muscle - a condition called sarcopenia. About 1 in 5 people with COPD develop it. And those who do are 20-40% more likely to die within five years than those without muscle loss. This isn’t just about being weak. It’s about losing the ability to walk, climb stairs, or even get out of a chair without help.
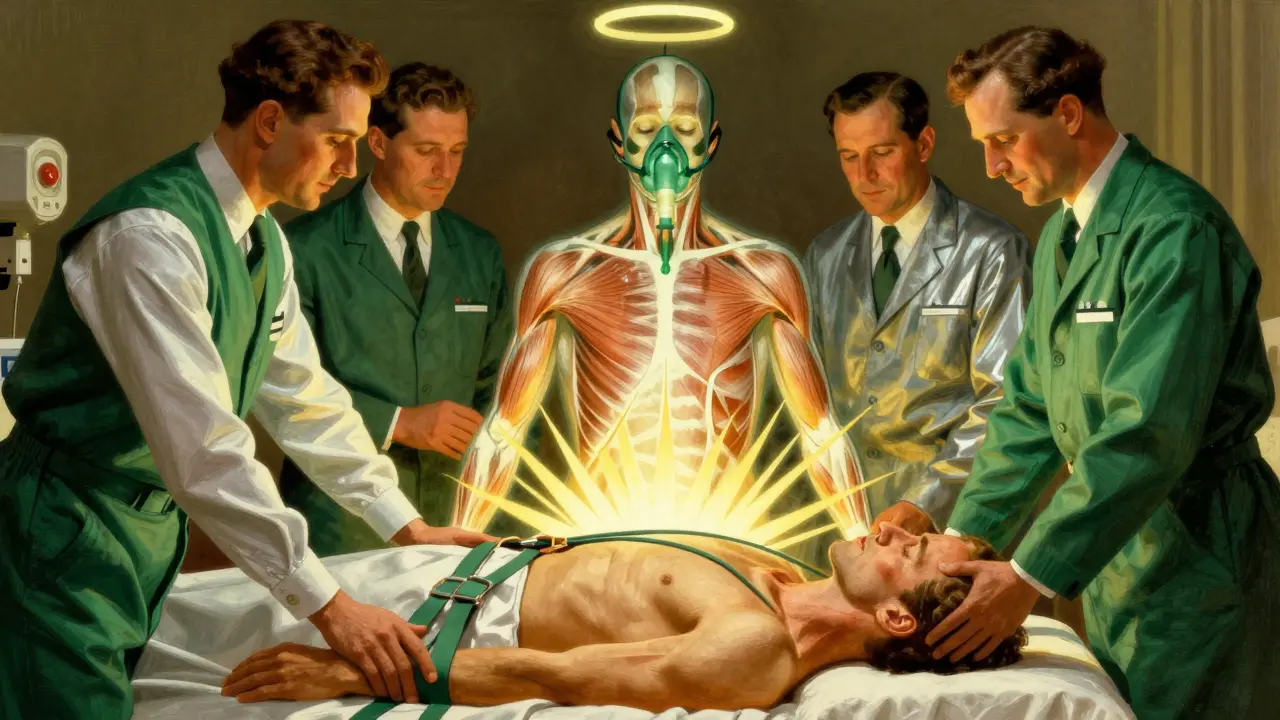
Sarcopenia in COPD isn’t the same as aging alone. In healthy older adults, muscle loss happens slowly, mostly in the legs. In COPD, it hits harder and faster - especially in the chest, arms, and breathing muscles. Studies show 68% of COPD patients have noticeable wasting in their pectoral muscles, compared to just 22% of people their age without lung disease. This isn’t random. It’s caused by a mix of low oxygen at night, constant inflammation, not moving enough, and not eating enough protein.
The good news? You can fight back. Research proves that combining the right nutrition with smart resistance training can reverse muscle loss, cut hospital stays by a third, and boost survival rates from 45% to nearly 70% in severe cases. But it has to be done right. Standard gym routines won’t work. And eating a normal diet won’t cut it either.
How sarcopenia is diagnosed in COPD patients
Doctors don’t just guess when someone has sarcopenia. There are clear, measurable signs - and they’re different for people with COPD than for the general population.
The first thing they check is muscle strength. For men, that means a handgrip strength below 27 kg. For women, below 16 kg. If that’s low, they move on to muscle mass. This is measured using a DEXA scan, which looks at lean tissue in the arms and legs. In COPD patients, the cutoffs are lower than normal: less than 7.0 kg/m² for men and 5.5 kg/m² for women.
But here’s the twist: many COPD patients are underweight or have low BMI, so standard muscle mass measurements miss the problem. That’s why doctors now use something called the pectoralis muscle index (PMI). It’s a CT scan of the chest at the third lumbar vertebra, measuring the size of the chest muscle relative to BMI. A PMI below 1.06 cm²/BMI is a red flag for sarcopenia in COPD - and it’s more accurate than BMI alone.
Finally, they test how well the person moves. The Short Physical Performance Battery (SPPB) looks at balance, walking speed, and how fast someone can stand up from a chair five times. A score below 8 means physical performance is severely impaired. If someone has low strength, low muscle mass, and low performance - that’s severe sarcopenia. And it’s linked to worse lung function. The lower the FEV1, the worse the muscle loss tends to be.
Why resistance training works - but only if it’s done correctly
Resistance training isn’t about lifting heavy weights. For someone with COPD and sarcopenia, it’s about moving safely, slowly, and consistently.
Most people think they need to lift 70-80% of their max to build muscle. But that’s too much for someone who gets out of breath just walking to the bathroom. Studies show the sweet spot is 30-40% of your one-rep max - that’s the lightest weight you can lift once. Start with resistance bands or 1-2 pound dumbbells. Do two sets of 10-15 reps, three times a week.
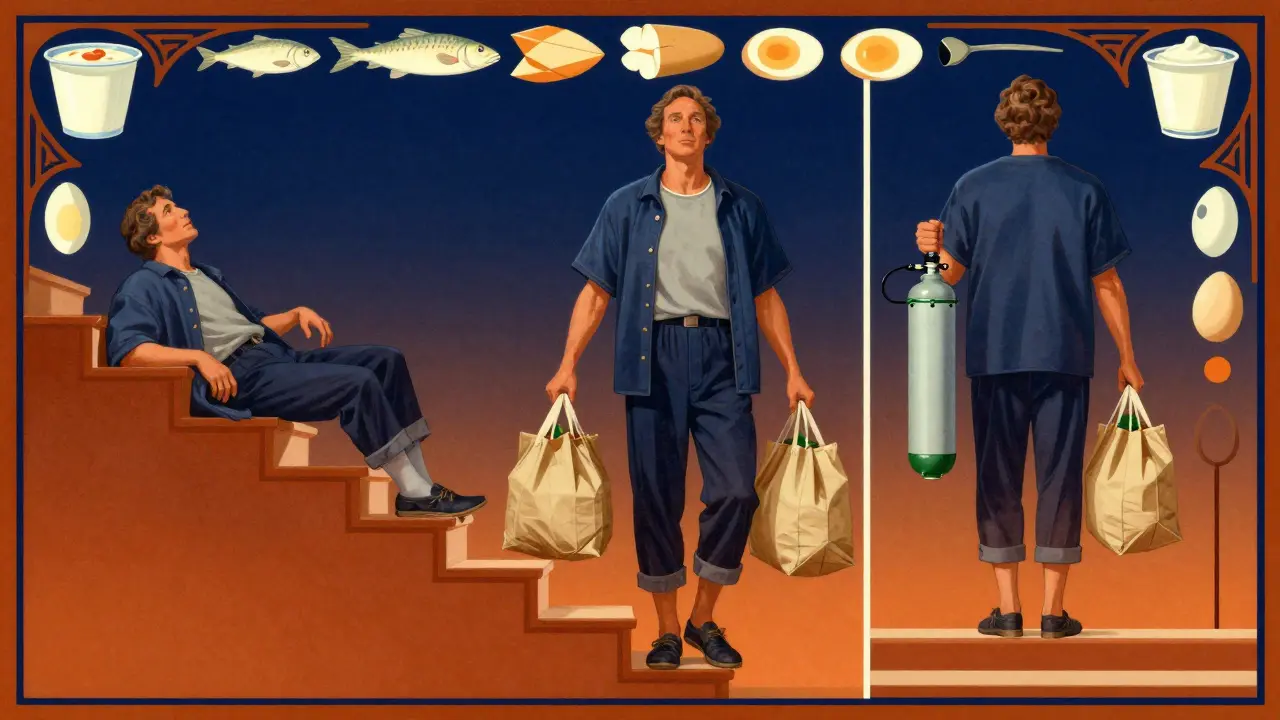
Rest is just as important as the workout. Take 2-3 minutes between sets. That gives your lungs time to recover. If you need oxygen during exercise - and 42% of COPD patients do - use it. Don’t skip it because you’re embarrassed. Supplemental oxygen during training cuts dyspnea by half and lets you do more reps.
Focus on big muscle groups: legs, chest, back, shoulders. Squats with support, seated rows with bands, wall push-ups, and seated shoulder presses are all safe. Don’t rush. Progress is slow. It takes 8-12 weeks to see real gains. But in one study from Cleveland Clinic, patients improved their 6-minute walk distance by 23% after 16 weeks of this approach.
And here’s the kicker: COPD patients who do resistance training get bigger strength gains than non-COPD sarcopenic patients. Why? Because their muscles are more responsive to stimulus when inflammation is controlled. It’s not magic - it’s science.
What to eat - and how much protein you really need
Most COPD patients eat about 0.9 grams of protein per kilogram of body weight per day. That’s the amount recommended for a healthy adult. But for someone with sarcopenia, it’s not enough. You need 1.2 to 1.5 grams per kg per day.
That means if you weigh 70 kg (about 154 lbs), you need 84 to 105 grams of protein daily. Most people spread that out over two meals - breakfast and dinner. But that’s the wrong way. Muscle building works best when protein is evenly spaced. Aim for 4 meals or snacks with 0.3-0.4 grams of protein per kg per meal. So for a 70 kg person, that’s 21-28 grams of protein every 4-5 hours.
Good sources? Eggs, Greek yogurt, cottage cheese, chicken, fish, tofu, and whey protein. Whey is especially helpful because it’s rich in leucine - an amino acid that turns on muscle growth. Adding 2.5-3.0 grams of leucine per meal boosts muscle synthesis by 37%. Many whey protein powders now include this amount. One scoop of a fortified supplement can give you 10 grams of leucine.
Don’t rely on appetite. In advanced COPD, people lose their hunger. That’s why liquid supplements work. A shake with 20-30 grams of protein and 3 grams of leucine between meals can make a huge difference. Try one after your morning walk, another mid-afternoon, and one before bed.
The hidden enemy: inflammation and low oxygen at night
It’s not just about food and exercise. There’s a deeper problem: inflammation and nighttime oxygen drops.
People with COPD and sarcopenia have higher levels of TNF-alpha and IL-6 - two inflammatory chemicals that break down muscle. Studies show these markers are strongly linked to weaker grip strength and less muscle mass. If you’re on long-term steroids for COPD, that can make it worse. Steroids reduce inflammation but also cause muscle wasting over time.
Then there’s nocturnal hypoxemia - low oxygen while you sleep. If your oxygen saturation drops below 88% for more than 30% of the night, your risk of severe sarcopenia jumps by 47%. That’s why home overnight oxygen therapy isn’t just for breathing - it’s for muscle preservation.
Ask your doctor for a sleep study if you’re not already doing one. If you’re on oxygen at night, make sure it’s set correctly. Many patients are on too low a flow. Even a small increase can help your muscles recover while you sleep.
What doesn’t work - and why people quit
Not everyone succeeds. About one-third of COPD patients stop resistance training because it makes their breathing worse. That’s not their fault. It’s often because the program wasn’t tailored.
Here’s what fails:
- Starting too heavy - lifting 5+ pound weights right away
- Not using oxygen during exercise
- Skipping protein between meals
- Trying to do it all at once - exercising daily instead of 2-3 times a week
- Stopping during flare-ups without a plan to restart
People also quit because they don’t see results fast enough. Muscle doesn’t rebuild overnight. It takes months. But small wins matter. One woman in a support group said she could carry groceries again after 12 weeks. Another said she stopped needing help to get dressed. These aren’t big feats - but they’re life-changing.
If you’ve tried and failed before, don’t give up. Try again - but this time, work with a pulmonary rehab specialist. They know how to adjust resistance, breathing techniques, and oxygen use. Most community centers don’t have trained staff. Academic hospitals do. Ask your doctor for a referral.
What’s next: new treatments on the horizon
The field is moving fast. In 2024, GOLD released the first official algorithm for managing sarcopenia in COPD. It links oxygen therapy, exercise intensity, and protein intake into one plan.
A major European trial (EU-SARC-COPD) is testing a supplement called HMB - a compound that helps muscles rebuild. Early results show it preserves muscle mass 18% better than placebo.
There’s also a new drug in phase 2 trials called PTI-501. It blocks myostatin - a protein that stops muscle growth. In early tests, it increased muscle mass in COPD patients without side effects. Results are expected in mid-2025.
But none of these are magic bullets. The best results still come from the basics: protein, resistance training, oxygen, and consistency. The future isn’t about pills. It’s about making these proven strategies part of everyday COPD care.
Real progress starts with one step
You don’t need to run a marathon or drink protein shakes every hour. Start small. Add one extra egg to breakfast. Do two minutes of seated leg lifts with a resistance band. Use your oxygen during walks. That’s it.
Track your progress: How many stairs can you climb now? Can you stand up from a chair without using your hands? Can you carry your own laundry? These are your real goals - not the number on a scale.
Sarcopenia in COPD is not inevitable. It’s not just a part of aging. It’s a treatable condition. And the tools to fight it are already here. You just need to use them - slowly, steadily, and with support.


Maggie Noe
January 10, 2026 AT 00:18Aron Veldhuizen
January 11, 2026 AT 22:44Meghan Hammack
January 12, 2026 AT 02:48Johanna Baxter
January 12, 2026 AT 08:11Jerian Lewis
January 13, 2026 AT 18:10tali murah
January 14, 2026 AT 09:45Jenci Spradlin
January 15, 2026 AT 21:19Micheal Murdoch
January 17, 2026 AT 12:55Drew Pearlman
January 17, 2026 AT 20:09Chris Kauwe
January 18, 2026 AT 06:26RAJAT KD
January 18, 2026 AT 17:57Lindsey Wellmann
January 19, 2026 AT 16:55Ian Long
January 20, 2026 AT 11:35Pooja Kumari
January 21, 2026 AT 02:41