Tacrolimus Neurotoxicity Risk Calculator
Based on factors from your transplant and current health status
Important Recommendations
When you get a transplant, the goal is simple: keep your new organ alive. But for many, that comes with a hidden cost - neurological side effects from the very drug meant to save you. Tacrolimus is one of the most powerful immunosuppressants out there, used in over 80% of kidney, liver, and heart transplants. It works better than older drugs like cyclosporine at preventing rejection. But for tacrolimus neurotoxicity, the trade-off is real. About 1 in 3 transplant patients will experience tremors, headaches, or worse. And here’s the twist: it can happen even when your blood levels are "in range."
What Tacrolimus Neurotoxicity Really Looks Like
Most people think side effects mean nausea or a rash. But with tacrolimus, the body often fights back through the nervous system. Tremor is the most common sign - affecting 65 to 75% of those who develop neurotoxicity. It’s not just a slight shake. Patients describe it as a constant, uncontrollable quiver in their hands, making it hard to hold a cup, button a shirt, or write their name. One patient on a transplant forum said, "I dropped my fork 12 times at dinner. My wife had to feed me." Headache is nearly as common, reported by 45 to 55% of affected patients. These aren’t ordinary headaches. They’re deep, pounding, and often unresponsive to ibuprofen or acetaminophen. Some patients compare them to migraines that never fade. One liver transplant recipient on Reddit wrote: "I had a headache for 6 weeks straight. My level was 7.4 ng/mL - perfectly normal. But my brain felt like it was under pressure." Other symptoms pile on: tingling in fingers or toes (paresthesia), trouble sleeping (insomnia), dizziness, confusion, or even slurred speech. In rarer cases, patients develop ataxia - losing coordination to the point they can’t walk straight - or worse, seizures or brain swelling (PRES). These are medical emergencies.Why Blood Levels Don’t Tell the Whole Story
Doctors rely on blood tests to monitor tacrolimus. The standard targets are 5-15 ng/mL for kidney transplants, 5-10 ng/mL for liver and heart. But here’s the problem: neurotoxicity doesn’t care about those numbers. A 2023 study in Annals of Transplantation found that 21.5% of patients with neurotoxicity had levels above 15 ng/mL. But - and this is critical - there was no significant difference in average levels between those who had symptoms and those who didn’t. Some patients developed tremors at 6 ng/mL. Others stayed symptom-free at 18 ng/mL. Why? Because blood levels don’t measure what’s happening in the brain. Tacrolimus crosses the blood-brain barrier, but everyone’s barrier is different. Some people naturally let more of the drug in. Others have genetic differences in how their liver breaks it down - especially those with the CYP3A5 gene variant. A 2021 study from the University of Toronto showed that patients with this variant had a 27% lower risk of neurotoxicity when dosed based on their genetics instead of weight or standard protocols.Organ Matters: Some Transplants Carry Higher Risk
Not all transplant recipients are equally at risk. Liver transplant patients face the highest chance of neurotoxicity - 35.7% according to data from the University of Pittsburgh. Kidney transplant patients see it in 22.4%, lung in 18.9%, and heart in 15.2%. Why? The liver is where tacrolimus is mostly metabolized. If the liver is new, or still healing, it can’t process the drug properly. That means more of it floats around, increasing brain exposure. Also, liver transplant patients often get multiple drugs at once - antibiotics, painkillers, sedatives - that can stack with tacrolimus. Drugs like linezolid, midazolam, or even common antibiotics like carbapenems can double the risk of seizures or confusion. One patient’s tremor disappeared after they stopped a single antibiotic they’d been given for a UTI.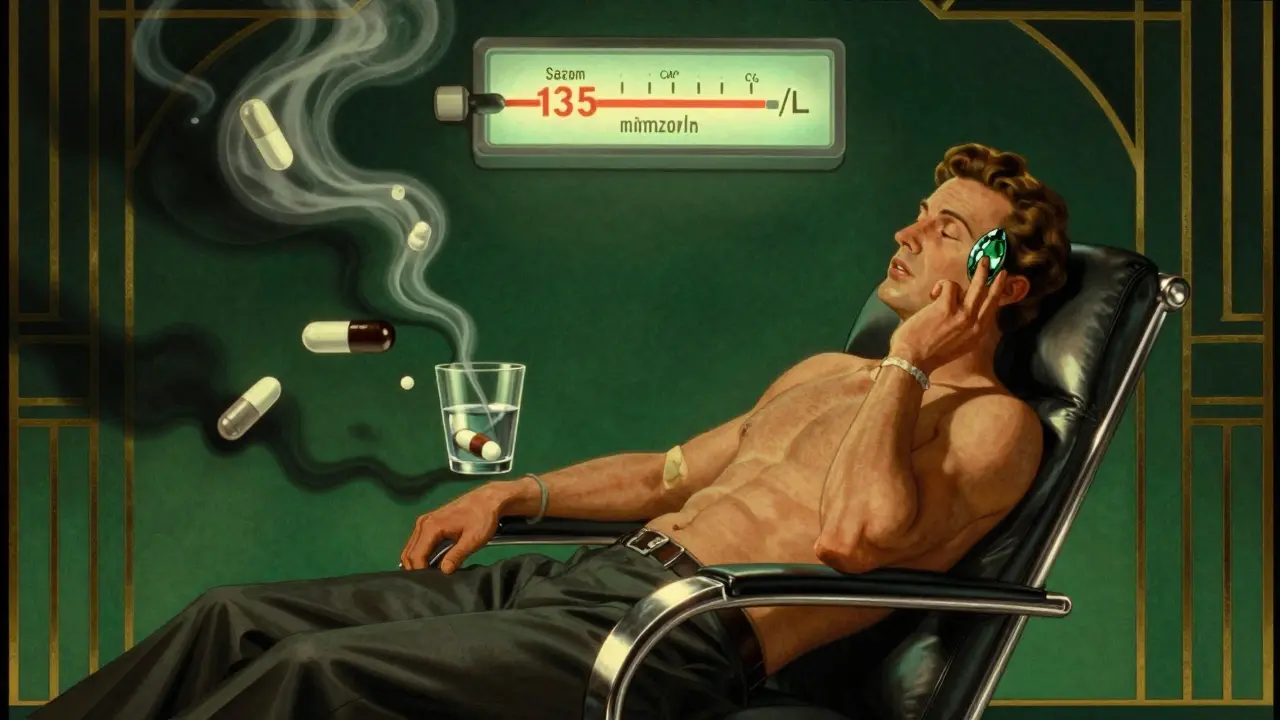
Electrolytes, Medications, and Hidden Triggers
It’s not just the drug itself. Low sodium (hyponatremia) is a major player. In 7 out of 12 studies reviewed, patients with sodium below 135 mmol/L had higher rates of neurotoxicity. Fixing the sodium level alone resolved symptoms in 28% of mild cases - without changing tacrolimus at all. Other hidden triggers? Stress, sleep deprivation, dehydration, or even a simple fever. The brain is sensitive. When your body is under stress, the blood-brain barrier gets leakier. That lets more tacrolimus in. It’s why many patients notice symptoms worsening during illness or after a night of poor sleep.What Doctors Do When Symptoms Show Up
Most transplant teams wait too long to connect the dots. A 2023 survey found 55% of patients waited 2-3 weeks before their doctors even considered tacrolimus as the cause. By then, symptoms are worse, and patients are more anxious. When neurotoxicity is suspected, there are three main moves:- Reduce the dose. Even a 10-20% drop can help. One patient reported tremors vanished within 72 hours after lowering their dose from 0.1 mg/kg to 0.07 mg/kg - while still staying within therapeutic range.
- Switch to cyclosporine. About 42% of patients are switched. Cyclosporine has a lower risk of tremor and headache (15-20% less), but it’s less effective at preventing rejection. About 15-20% more patients reject their grafts after switching.
- Check for drug interactions. If you’re on antibiotics, antifungals, or antipsychotics, ask if they could be making things worse.

What’s Changing in 2026
The field is waking up. In 2023, the American Society of Transplantation released its first-ever guidelines specifically for managing neurotoxicity. They now recommend routine neurological checks in the first 30 days after transplant - not just blood tests. The biggest shift? Personalized dosing. Instead of guessing based on weight, doctors are starting to test for CYP3A5 gene variants. Those with the "fast metabolizer" type can handle higher doses without side effects. Those with the "slow" type need lower doses from day one. This approach is still rare - mostly in academic centers - but it’s growing. A new trial called TACTIC, launching in 2024, is testing a smarter algorithm that combines genetics, magnesium levels, blood pressure, and tacrolimus concentration to predict and prevent neurotoxicity before it starts. Early results look promising. And in the background, a new drug called LTV-1 is in phase 2 trials. Designed to stay out of the brain, it could replace tacrolimus entirely by 2027 - if it works.What You Should Do
If you’re on tacrolimus and notice:- Shaking hands you can’t stop
- Headaches that don’t go away
- Confusion, dizziness, or trouble speaking
- "Could this be from tacrolimus?"
- "Have you checked my sodium and magnesium?"
- "Am I on any other drugs that could make this worse?"
- "Could we test my CYP3A5 gene?"
Can tacrolimus neurotoxicity happen even if my blood level is normal?
Yes. Blood levels between 5-15 ng/mL are considered therapeutic, but neurotoxicity can occur at any level. Some patients develop tremors or headaches at 6 ng/mL, while others tolerate 18 ng/mL without symptoms. This is because individual differences in brain barrier permeability, genetics (like CYP3A5), and other medications affect how much tacrolimus enters the brain - not just how much is in the blood.
Which transplant recipients are most at risk for tacrolimus neurotoxicity?
Liver transplant recipients have the highest risk - about 35.7% experience neurotoxic symptoms. This is likely because the liver metabolizes tacrolimus, and a new or healing liver may not process the drug properly, leading to higher brain exposure. Kidney transplant patients have a 22.4% risk, lung at 18.9%, and heart at 15.2%.
Can low sodium make tacrolimus neurotoxicity worse?
Yes. Hyponatremia (serum sodium below 135 mmol/L) is a known risk factor. Studies show that correcting low sodium alone resolved mild neurotoxicity in 28% of cases without needing to change the tacrolimus dose. The brain is sensitive to salt balance, and low sodium may increase blood-brain barrier permeability, letting more tacrolimus in.
Are there drugs that make tacrolimus neurotoxicity worse?
Yes. Several medications can increase the risk, including linezolid, carbapenem antibiotics, midazolam, propofol, haloperidol, lorazepam, risperidone, and olanzapine. These drugs can lower the seizure threshold or interfere with how tacrolimus is processed. Always review all your medications with your transplant team - even short-term antibiotics or sleep aids.
Is there a genetic test that can help prevent neurotoxicity?
Yes. Testing for the CYP3A5 gene variant can predict how your body breaks down tacrolimus. People with the "fast metabolizer" genotype clear the drug more quickly and can often tolerate higher doses without side effects. Those with the "slow" variant are at higher risk of toxicity. A 2021 study showed that using this test to guide dosing reduced neurotoxicity by 27%. While not yet standard everywhere, it’s becoming more common in transplant centers.


Joshua Smith
February 8, 2026 AT 11:40I've been on tacrolimus for 4 years post-kidney transplant, and honestly, the tremors were the worst part. Not the nausea, not the fatigue - just this constant shaking in my hands that made typing feel impossible. I didn't connect it to the drug until my nurse mentioned it during a routine check. Turns out, my sodium was low from drinking too much water trying to 'stay healthy.' Fixing that alone cut my tremors in half. No dose change needed.
Just a reminder: sometimes the fix isn't more meds - it's checking the basics. Sodium, sleep, hydration. They matter more than we think.