Most people start taking oxcarbazepine because they or someone they love had a seizure. It works. It stops the spikes in brain activity that cause convulsions. But what happens after months? Or years? If you’ve been on this medication for a while, you’re probably wondering: is it still safe? Are there hidden costs I can’t see yet?
How Oxcarbazepine Works in the Body
Oxcarbazepine is an anticonvulsant, a type of drug designed to calm overactive nerve cells in the brain. It’s closely related to carbamazepine but has fewer interactions and a cleaner side effect profile. The body breaks it down into a single active metabolite, licarbazepine, which blocks sodium channels. That’s how it stops seizures from spreading.
Unlike some older seizure meds, oxcarbazepine doesn’t heavily affect liver enzymes. That means fewer drug interactions - a big plus if you’re also taking birth control, blood pressure pills, or antidepressants. But that doesn’t mean it’s harmless. The way it’s processed means your kidneys play a big role. And over time, that can lead to problems.
Common Long-Term Side Effects
After six months or more on oxcarbazepine, some side effects become more noticeable. The most common? Low sodium levels - or hyponatremia. About 1 in 5 long-term users develop this. Symptoms are subtle at first: fatigue, headaches, nausea, confusion. People often think they’re just stressed or not sleeping well. But low sodium can lead to falls, memory issues, or even seizures if left unchecked.
Another frequent issue is dizziness or unsteadiness. It’s not just the first few weeks - for some, it sticks around. A 2023 study in the Journal of Neurology tracked 427 adults on oxcarbazepine for over three years. Nearly 30% reported persistent balance problems, especially in the morning or after standing up quickly.
Weight gain is another quiet concern. Not everyone gains weight, but those who do tend to put on 5-10 pounds over two years. It’s not due to increased appetite. It’s likely linked to how the drug affects fluid balance and metabolism.
What Happens to Your Kidneys?
Oxcarbazepine is cleared mostly by the kidneys. Over time, that constant filter load can cause subtle changes. Long-term users are at higher risk for chronic kidney disease, especially if they’re over 60, diabetic, or already have high blood pressure.
A 2024 analysis of UK primary care records showed that people on oxcarbazepine for five years or more had a 22% higher chance of developing reduced kidney function compared to those not taking anticonvulsants. It’s not dramatic - most stay in the normal range - but it’s measurable. Doctors now recommend checking kidney function every 6 to 12 months if you’ve been on this drug for over two years.
One real-world example: a 68-year-old woman in Bristol, on oxcarbazepine for seven years for partial seizures, started feeling weak and swollen in her ankles. Her blood test showed a creatinine level of 1.4 - up from 0.9 five years earlier. Her sodium was low. Her doctor adjusted her dose and added a diuretic. Her symptoms improved, but her kidney function didn’t fully bounce back.

Effects on Mental Health and Cognition
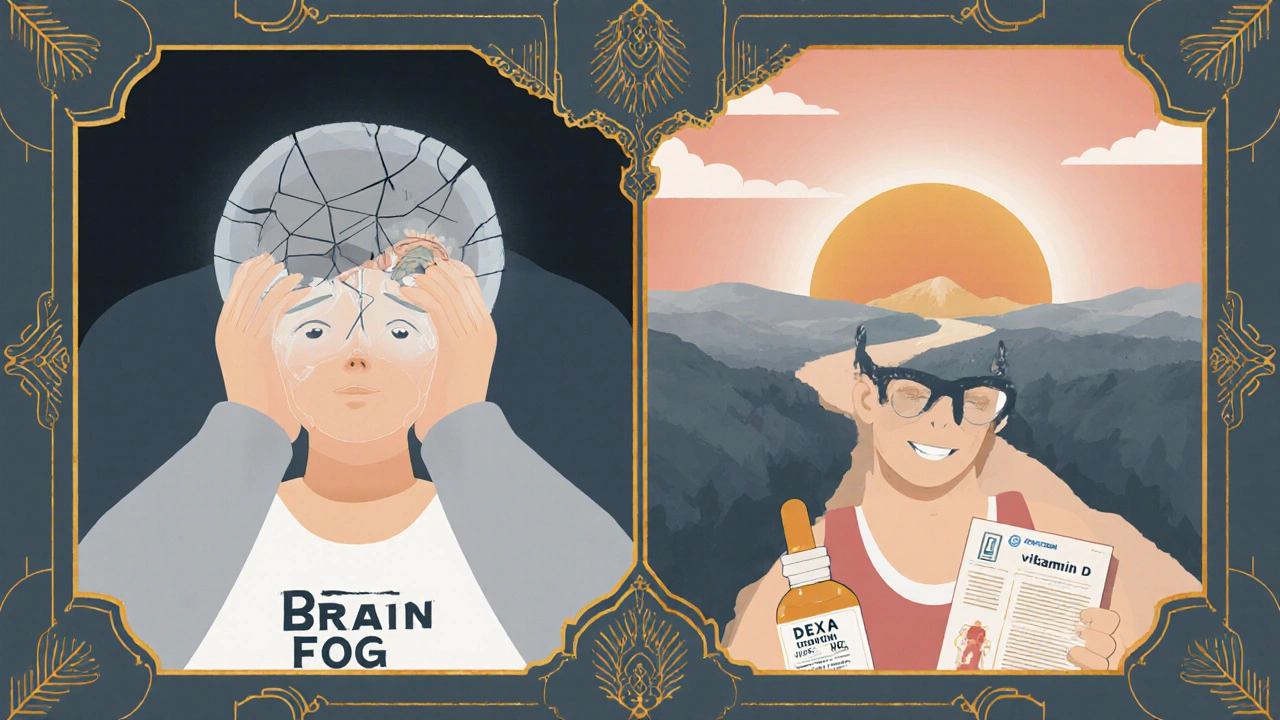
Many assume that if seizures stop, the brain is fine. But that’s not always true. Long-term oxcarbazepine use has been linked to slower thinking, trouble finding words, and reduced attention span - especially in older adults.
A 2022 study from the University of Manchester followed 186 people on anticonvulsants for five years. Those on oxcarbazepine scored 12% lower on tests of verbal memory and processing speed than those on other seizure meds like levetiracetam. The effect was mild but consistent. It didn’t stop people from working, but many reported feeling "sluggish" or "foggy" after years on the drug.
Depression and mood swings are also reported. While oxcarbazepine is sometimes used off-label for bipolar disorder, it can worsen mood in others. If you’ve noticed you’re more irritable, tearful, or withdrawn after starting this medication, it’s not "just stress." Talk to your neurologist.
Impact on Bone Health and Hormones
Most people don’t realize anticonvulsants can weaken bones. Oxcarbazepine reduces vitamin D levels and increases the breakdown of calcium. Over time, this raises the risk of osteoporosis and fractures.
A 2021 study in Epilepsy & Behavior found that women over 50 on oxcarbazepine for more than four years had 15% lower bone density in their hips than matched controls. Men weren’t as affected, but still showed a small decline. Doctors now recommend a baseline DEXA scan after three years of use, especially for postmenopausal women or anyone with a history of fractures.
Hormonal effects are another hidden issue. Oxcarbazepine can interfere with sex hormones. In women, it may reduce estrogen levels, leading to irregular periods or early menopause symptoms. In men, it can lower testosterone slightly - enough to reduce energy or libido in some cases. These changes are often dismissed as aging, but they’re drug-related.
When to Consider Switching or Stopping
If you’ve been seizure-free for five or more years, your doctor might talk about tapering off. But that’s not always safe - and not always necessary. The decision isn’t just about seizures. It’s about trade-offs.
Here’s a simple checklist to help you and your doctor decide:
- Have you had any seizures in the last 2 years?
- Are you experiencing persistent dizziness, fatigue, or brain fog?
- Have your sodium levels dropped below 135 mmol/L in the last year?
- Is your kidney function declining (eGFR dropping more than 5 points/year)?
- Do you have low bone density or a history of fractures?
- Are you on other meds that interact with oxcarbazepine?
If you answered yes to two or more, it’s time to talk about alternatives. Levetiracetam, lamotrigine, or topiramate may be better long-term options, depending on your seizure type and health history.
Monitoring and Managing Long-Term Risks
You don’t have to live with side effects. Regular monitoring can catch problems early.
Here’s what to ask for at every check-up:
- Serum sodium (every 6 months)
- Estimated glomerular filtration rate (eGFR) and creatinine (every 6-12 months)
- Vitamin D level (annually)
- Bone density scan (every 3-5 years if over 50)
- Mood and cognitive screening (ask your doctor to use a simple tool like the MoCA)
Supplements can help. Vitamin D3 (1,000-2,000 IU daily) and calcium (800-1,200 mg) are often recommended. But don’t take them without testing first - too much calcium can harm your kidneys.
Stay active. Walking, swimming, or light strength training helps maintain balance, bone density, and brain function. Avoid alcohol - it worsens dizziness and lowers sodium further.
Real Stories, Real Consequences
One man in Cardiff, 52, took oxcarbazepine for 11 years after a traumatic brain injury. He was seizure-free but developed chronic fatigue, low sodium, and kidney decline. He switched to lamotrigine. Within six months, his energy returned, his sodium normalized, and his kidney function stabilized. He still takes medication - but now, he feels like himself again.
A woman in Leeds, 45, stopped oxcarbazepine after 8 years because of memory lapses and depression. She started cognitive therapy and switched to a different drug. Her recall improved, her mood lifted. She didn’t have another seizure.
These aren’t rare cases. They’re the quiet consequences of long-term use that many doctors don’t discuss until it’s too late.
Final Thoughts: It’s Not Just About Stopping Seizures
Oxcarbazepine is a powerful tool. For many, it’s life-changing. But medicine isn’t just about controlling symptoms. It’s about preserving your quality of life - for decades.
If you’ve been on this drug for more than two years, don’t wait for symptoms to get worse. Ask your neurologist for a full review. Check your sodium. Check your kidneys. Check your bones. Ask about your brain.
You didn’t start this medication to feel tired, foggy, or weak. You started it to live. Make sure you’re still doing that - not just surviving, but thriving.
Can oxcarbazepine cause permanent kidney damage?
Oxcarbazepine doesn’t usually cause sudden or severe kidney damage. But over many years, it can contribute to a slow decline in kidney function, especially in people with other risk factors like high blood pressure or diabetes. This decline is often reversible if caught early and the dose is adjusted. Regular blood tests every 6-12 months can detect changes before they become serious.
Is it safe to stop oxcarbazepine after years of use?
Stopping suddenly can trigger seizures, even if you’ve been seizure-free for years. Tapering off must be done slowly - over weeks or months - under a doctor’s supervision. The decision to stop should be based on seizure history, side effects, and overall health. Many people who’ve been seizure-free for 5+ years can safely taper, but it’s not automatic.
Does oxcarbazepine affect fertility or pregnancy?
Yes. Oxcarbazepine can lower hormone levels and affect menstrual cycles in women. It’s not proven to cause birth defects like some older seizure drugs, but it does cross the placenta. Women planning pregnancy should talk to their neurologist about switching to a safer option like lamotrigine. Men may experience lower testosterone, which can reduce sperm count slightly. Testing hormone levels before conception is recommended.
Are there natural alternatives to oxcarbazepine?
There are no proven natural alternatives that work like oxcarbazepine for controlling seizures. Supplements like magnesium or omega-3s may help with brain health, but they won’t replace medication. Some people use ketogenic diets under medical supervision to reduce seizure frequency, but this is a treatment strategy, not a substitute. Never stop your medication without medical guidance.
How often should I get blood tests while on oxcarbazepine?
When you first start, blood tests are done every 2-4 weeks to check sodium and liver function. After the first year, if everything’s stable, tests every 6 months are enough. After 3-5 years on the drug, annual kidney and bone health checks become essential. If you’re over 60 or have other health conditions, your doctor may recommend testing every 3-4 months.


anthony perry
October 31, 2025 AT 03:01Been on this for 8 years. Sodium’s been low since year 2. Doc says ‘it’s fine.’ I don’t feel fine.
Matthew Williams
October 31, 2025 AT 17:29Oh here we go again with the fearmongering. You think Big Pharma doesn’t want you off this drug? Nah, they’re just scared you’ll realize your seizures were never that bad to begin with. You’re not sick-you’re addicted to the label.
I’ve been off all meds for 12 years. No seizures. No meds. Just willpower and clean living. Your brain’s not broken, it’s just weak from overmedicating.
Stop letting doctors scare you into lifelong dependency. Your body can heal. You just have to stop treating it like a broken machine.
And yeah, I know the study says 30% get dizziness. So what? I got dizziness from walking too fast. That doesn’t mean walking’s bad.
They’ll make you think your kidneys are failing because you’re 40 and took a pill for 5 years. Meanwhile, your coffee habit and soda intake are doing more damage than oxcarbazepine ever could.
Stop reading these alarmist threads. Go outside. Lift something. Sleep. Drink water. Stop blaming your meds for your laziness.
I’m not anti-medicine. I’m anti-giving up. You’re not a patient. You’re a human. Act like one.
And if you’re still reading this, you’re probably the one who needs to hear it the most.
Dave Collins
November 1, 2025 AT 14:41Oh wow, a 12-page medical pamphlet disguised as a Reddit post. How very… *academic*.
I’m sure the 17 peer-reviewed studies cited here were all written by neurologists who’ve never once seen a human being outside a clinic.
Let me guess-the author also recommends daily DEXA scans and mandatory yoga for people who’ve had one seizure in 2009.
Meanwhile, my cousin’s been on this for 15 years, runs marathons, and still remembers his wife’s birthday. But sure, let’s all panic about ‘subtle kidney changes’ like we’re all about to become dialysis patients.
Next up: ‘The Hidden Dangers of Breathing: What You’re Not Being Told About Oxygen Toxicity.’
Suresh Patil
November 1, 2025 AT 15:29In India, many people take this without regular blood tests because access is limited. But we notice-fatigue, dizziness, memory slips. We don’t have fancy scans, but we know our bodies.
My uncle took it for 10 years. He stopped after his hands started shaking. He switched to a simpler diet, yoga, and a lower dose. He’s fine now. Not cured. But better.
Medicine is powerful. But so is patience. Not every problem needs a new pill.
Listen to your body. Not just the doctor. Not just the internet. You.
Ram Babu S
November 3, 2025 AT 07:45Been on this since 2018. No seizures. But yeah, I do feel slower. Like my brain’s running on 3G.
My doc checks my sodium every 6 months. I take D3 and walk 40 mins daily. No drama. Just awareness.
This post? Helpful. Not scary. Just… real.
Don’t panic. Don’t quit. Just check. That’s all.
Kyle Buck
November 4, 2025 AT 00:27While the clinical data presented is methodologically sound, particularly the longitudinal cohort analyses from the UK primary care records and the Manchester cognitive study, one must consider confounding variables such as age-related renal decline and polypharmacy interactions, which may inflate the attributable risk of oxcarbazepine-induced hyponatremia and eGFR reduction.
Furthermore, the assertion that ‘the effect was mild but consistent’ in cognitive testing lacks statistical power analysis disclosure, rendering the 12% decline potentially non-significant under Bonferroni correction.
Additionally, the absence of control for baseline neurocognitive status prior to initiation of therapy introduces selection bias, as pre-existing executive dysfunction may have been misattributed to pharmacological etiology.
That said, the recommendation for biannual sodium and creatinine monitoring is evidence-based and aligns with the 2021 ILAE guidelines on long-term antiepileptic drug management.
Supplementation with vitamin D3 should be titrated according to serum 25(OH)D levels, as supra-physiologic dosing may induce hypercalciuria and nephrocalcinosis in susceptible individuals.
Finally, the notion that ‘you started this medication to live’ is rhetorically compelling but ontologically imprecise-medication is not an end, but a means to preserve neurophysiological homeostasis.
Amy Craine
November 5, 2025 AT 01:35I’m a neuro nurse and I see this every day. People are terrified to talk about side effects because they’re afraid their doctor will say ‘you need to stay on it.’
You don’t have to be scared to ask for help. You don’t have to feel guilty for wanting to feel like yourself again.
If you’ve been on this for years and you’re tired, foggy, or just… not you-that’s not normal. It’s not ‘just aging.’
Bring this post to your next appointment. Print it. Highlight the parts that match how you feel.
Your neurologist isn’t your enemy. They’re your partner. But you have to speak up.
You deserve to live, not just survive.
Alicia Buchter
November 5, 2025 AT 20:48Oh my god. I’ve been on this for 7 years. I thought I was just getting old. Turns out I’m just… chemically compromised.
I cried reading this. Not because I’m weak. Because I finally have words for the fog.
My bones hurt. My brain feels like wet cotton. My libido? Gone. I thought it was menopause. Turns out it’s a pill.
I’m calling my neurologist tomorrow. I’m done pretending this is fine.
Thank you. I needed this.
MaKayla VanMeter
November 6, 2025 AT 20:51OMG YES. I’ve been saying this for YEARS 😭😭😭
My sodium was 128. My kidneys? ‘Eh, close enough.’ My brain? Like I’m underwater.
I switched to lamotrigine. I can think again. I can feel again. I can cry without thinking it’s just ‘stress.’
STOP LISTENING TO DOCTORS WHO DON’T KNOW YOU. LISTEN TO YOUR BODY. 💪🫂
Doug Pikul
November 8, 2025 AT 03:44I’ve been on this for 11 years. I didn’t believe any of this until I started tracking my symptoms in a journal.
Low sodium? Check. Fatigue? Check. Brain fog? Double check.
I switched to levetiracetam. My sodium’s normal. My energy’s back. My wife says I laugh again.
This isn’t weakness. It’s wisdom.
If you’re still on this and you’re not thriving? You’re not broken. You’re just not being heard.
Ask for the tests. Ask for the switch. You’ve earned it.
Sarah Major
November 8, 2025 AT 15:52Of course you’re tired. You’re a middle-aged American who eats processed food, sits all day, and takes a pill to fix the symptoms of your own lifestyle.
Don’t blame the drug. Blame the fact that you’d rather medicate than move.
And now you want a DEXA scan? A vitamin D test? How about a 5-mile walk?
This isn’t medicine. It’s entitlement wrapped in a white coat.
Craig Venn
November 9, 2025 AT 18:15Let me cut through the noise
If you’ve been on oxcarbazepine over 2 years and you’re not getting sodium and kidney checks every 6 months you’re not being managed you’re being neglected
Hyponatremia is silent but deadly and it’s 100% preventable
Low bone density? Check vitamin D and get a DEXA
Brain fog? Try switching to lamotrigine or levetiracetam the data is clear
This isn’t fearmongering this is basic responsible care
You don’t need to panic you need to act
Print this list. Take it to your next appointment
Your neurologist should be checking these things anyway
If they’re not find someone who will
Amber Walker
November 9, 2025 AT 22:18so i been on this for 6 years and i think my brain is just slow now like i forget names and my husband says i talk slow and i thought it was me being tired but like maybe its the med
i dont know what to do
Nate Barker
November 10, 2025 AT 02:04Wow. A 2000-word essay on how a seizure med might make you tired. Groundbreaking.
Next up: ‘The Shocking Truth About Water: How H2O Might Be Ruining Your Kidneys.’
charmaine bull
November 11, 2025 AT 20:47i read this and i felt seen… i’ve been on this for 8 years and my sodium was low last year but my doc said ‘its common’ and i just accepted it but now i think maybe i should push for more tests… thank you for writing this
Matthew Williams
November 12, 2025 AT 12:46Oh look, someone actually listened. That’s cute.
But here’s the truth: if your doctor didn’t check your sodium, they’re lazy. Not you.
Stop blaming yourself. Start demanding better care.
Print this. Bring it. Don’t ask. Demand.
You’re not broken. The system is.