Vancomycin Risk Assessment Calculator
Enter patient-specific factors to assess the risk of vancomycin-induced nephrotoxicity and ototoxicity, and get dosing recommendations based on current guidelines.
For optimal safety, use this tool to guide your vancomycin dosing decisions and monitoring schedule.
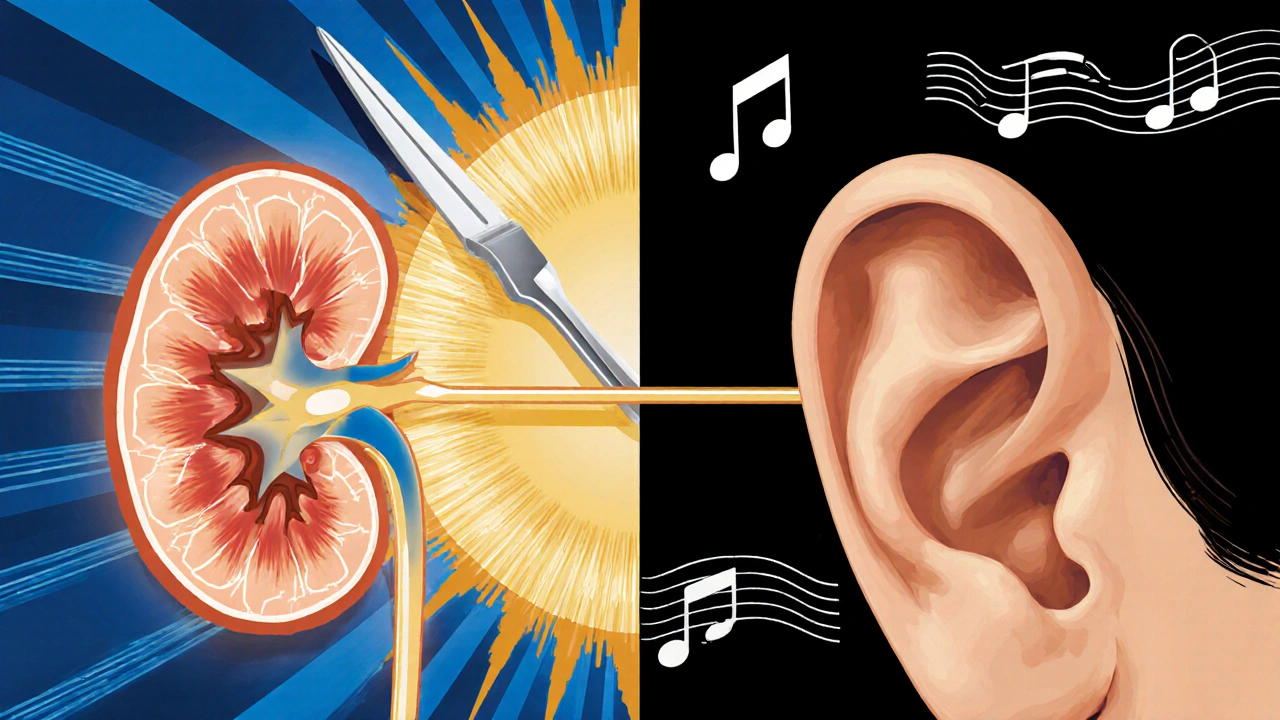
Vancomycin saves lives. It’s one of the few antibiotics that can stop MRSA when nothing else works. But every time you give it, you’re walking a tightrope. On one side: nephrotoxicity - kidney damage that’s common but often reversible. On the other: ototoxicity - hearing loss that’s rare but permanent. You can’t avoid one without risking the other. The question isn’t whether vancomycin is dangerous - it’s how to use it without breaking your patient.
Why Vancomycin Still Matters
Vancomycin isn’t new. It’s been around since the 1950s. But it’s still the go-to for serious Gram-positive infections like MRSA, endocarditis, and complicated skin abscesses. Why? Because alternatives like daptomycin or ceftaroline don’t work as well in every situation. In fact, 89% of infectious disease specialists say vancomycin is still essential. But that doesn’t mean it’s safe. The old versions were messy - impurities caused kidney damage in over half of patients. Modern purification fixed that. But the risks didn’t disappear. They just changed shape.Nephrotoxicity: The More Common Threat
About 15 to 30% of patients on vancomycin develop kidney injury. That’s not rare. That’s expected in high-risk groups. The good news? Most cases are mild and bounce back once you stop the drug. The bad news? It’s happening more often than we thought - especially when vancomycin is mixed with piperacillin-tazobactam. A 2022 study of over 14,500 patients found that combination increases the risk of acute kidney injury by more than double compared to vancomycin with meropenem. What makes it worse? High doses. Doses over 4 grams a day triple the risk. High trough levels - above 15-20 mcg/mL - are a red flag. So is age, dehydration, pre-existing kidney disease, and being in the ICU. The damage? It’s direct. Vancomycin clings to the tubules in the kidneys, causes oxidative stress, and messes with the cells’ energy supply. You won’t see it right away. It usually shows up between day 3 and day 14. That’s why checking creatinine every 48 to 72 hours isn’t optional. It’s basic.Ototoxicity: The Silent Killer
Ototoxicity is different. It’s rare - maybe 1 to 3% of patients. But when it hits, it’s devastating. Bilateral, high-frequency hearing loss. Tinnitus. Sometimes, total deafness. And here’s the kicker: it can happen even with normal kidney function and normal trough levels. A 2023 case report showed hearing loss after just three doses. No warning. No elevated creatinine. Just silence. The mechanism? Vancomycin attacks the hair cells in the inner ear. Unlike the kidneys, the ear has no backup. Once those cells die, they don’t come back. And there’s no blood test for it. No early warning sign. Audiograms are the only way to catch it before it’s too late. But only 37% of hospitals even have protocols for that. Most rely on patients reporting ringing in their ears - which often happens too late.
The Trough Level Myth
For years, doctors chased trough levels of 15-20 mcg/mL, thinking higher meant better killing power. That was the old way. Now we know: above 15 mcg/mL, the risk of kidney damage spikes. But the antibacterial effect? It plateaus around 10 mcg/mL. That’s why the 2020 ASHP guidelines dropped the target to 10-15 mcg/mL for most infections. Lower troughs = less kidney damage. Same cure rates. But here’s the twist: ototoxicity doesn’t care about troughs. It’s tied to peak levels and total exposure. A patient with normal troughs can still get hearing loss if their peaks hit 80 mcg/mL or higher. That’s why monitoring only troughs is like checking the fuel gauge and ignoring the speedometer. You’re missing half the picture.Combination Therapy: The Hidden Trap
Vancomycin + piperacillin-tazobactam is everywhere. It’s the default for sepsis, pneumonia, abdominal infections. But it’s also the fastest route to kidney injury. The 2022 meta-analysis showed a 1.31-fold increase in AKI risk. That’s not a small bump. That’s a cliff. And here’s the irony: patients on this combo don’t die more often. They just spend more time in the hospital - an extra 3.2 days on average - and need dialysis more frequently. Yet, many still use it because it’s convenient. That’s not evidence-based. That’s habit. Some hospitals have started putting electronic alerts in their systems. If a doctor orders vancomycin and piperacillin together, the system flags it. One study showed that cut usage by 22%. Simple. Effective. Why isn’t this everywhere?Who’s at Highest Risk?
Not everyone gets hurt the same way. Some patients are walking targets.- Nephrotoxicity high-risk: Age over 65, pre-existing kidney disease, ICU stay, sepsis, daily vancomycin dose over 4g, concurrent aminoglycosides or NSAIDs, dehydration.
- Ototoxicity high-risk: Age over 65, pre-existing hearing loss, prolonged therapy (>7 days), daily dose over 4g, concomitant ototoxic drugs (like loop diuretics), genetic risk variants (like MT-RNR1 mutations).

Monitoring: What Actually Works
For kidneys: Check creatinine every 48-72 hours. More often if they’re sick or getting high doses. Watch for a 0.3 mg/dL rise in creatinine or a 50% drop in urine output. That’s AKI by the book. For ears: Baseline audiogram before starting. Repeat weekly if therapy lasts more than 7 days or if dose exceeds 4g/day. That’s the recommendation from the American Speech-Language-Hearing Association. But guess what? Most hospitals don’t do it. It’s expensive. It takes time. Audiologists are scarce. But the cost of ignoring it? Permanent hearing loss. Rehabilitation. Cochlear implants. Up to $50,000 a year per patient. Is skipping the audiogram really cheaper? There’s a better way: AUC monitoring. Instead of just checking trough levels, we measure the total drug exposure over time - area under the curve. A 2023 trial showed AUC-guided dosing cut nephrotoxicity from 18.7% to 9.4%. No increase in treatment failure. Just smarter dosing. Tools like DoseMeRx and PrecisePK are making this easier. Over 1,200 U.S. hospitals are already using them.The Bottom Line: How to Use Vancomycin Safely
You don’t need to avoid vancomycin. You need to use it smarter.- Use the lowest effective dose. Don’t chase 20 mcg/mL troughs. Aim for 10-15.
- Avoid vancomycin + piperacillin-tazobactam unless absolutely necessary. Use meropenem or another beta-lactam instead.
- Check creatinine every 2-3 days. Stop or switch if kidney function drops.
- For patients on high doses or long courses, get a baseline audiogram. Repeat if therapy goes beyond 7 days.
- Use AUC monitoring if you can. It’s more accurate than troughs alone.
- Know your patient’s risk factors. Age, kidney history, other drugs - they matter more than you think.
What’s Next?
The future of vancomycin isn’t about bigger doses. It’s about precision. Pharmacogenomics is identifying people who are genetically prone to ototoxicity. Point-of-care audiometers are being developed so nurses can check hearing at the bedside. New formulations are in the works - ones that target bacteria without touching the ear or kidney. But until then, the job hasn’t changed. You’re still balancing a life-saving drug against two silent, potentially devastating side effects. One is common. One is rare. But one can ruin a life forever.Don’t treat vancomycin like it’s just another antibiotic. Treat it like a scalpel - sharp, powerful, and dangerous if used carelessly.
Can vancomycin cause hearing loss even with normal kidney function?
Yes. While vancomycin ototoxicity was once thought to only happen in patients with kidney failure, modern case reports show it can occur even in people with perfectly normal kidney function. A 2023 report documented irreversible hearing loss after just three doses in a patient with no prior kidney or hearing issues. This suggests individual susceptibility - possibly genetic - plays a major role.
Is vancomycin nephrotoxicity reversible?
In most cases, yes. If caught early and vancomycin is stopped or the dose is reduced, kidney function usually returns to baseline within days to weeks. However, in patients with multiple risk factors - like sepsis, old age, or pre-existing kidney disease - the damage can be more severe and may require dialysis or lead to long-term chronic kidney disease.
Why is vancomycin still used if it’s so toxic?
Because for serious Gram-positive infections like MRSA, there are few reliable alternatives. Drugs like daptomycin or linezolid don’t work as well in all situations - especially for endocarditis, osteomyelitis, or infections in patients with poor gut absorption. Vancomycin remains the most widely studied and effective option for these cases. The key isn’t avoiding it - it’s using it correctly.
What’s the best way to monitor vancomycin levels?
Trough-only monitoring is outdated. The best approach is AUC-guided dosing - measuring the total drug exposure over 24 hours. Studies show AUC monitoring reduces nephrotoxicity by nearly half compared to traditional trough checks. It’s more accurate, especially for patients with fluctuating kidney function. Tools like DoseMeRx and PrecisePK make this feasible in most hospitals.
Should all patients get audiograms before vancomycin?
Not all - but high-risk patients should. That includes people over 65, those with prior hearing loss, those getting doses over 4 grams per day, or those on other ototoxic drugs like furosemide. For these patients, a baseline audiogram before starting and weekly repeats are recommended. While resource-heavy, the cost of untreated hearing loss far outweighs the cost of testing.
How long does it take for vancomycin to damage the kidneys?
Kidney damage usually shows up between day 3 and day 14 of therapy. That’s why checking creatinine every 48-72 hours is critical. Waiting longer than that risks missing early signs. The longer you wait, the harder it is to reverse.
Can vancomycin ototoxicity be prevented?
You can’t prevent it entirely, but you can reduce the risk. Keep doses as low as possible. Avoid prolonged therapy. Use AUC monitoring to avoid high peak levels. Avoid combining it with other ototoxic drugs. Get audiograms for high-risk patients. And know your patient’s genetics - emerging research shows certain gene variants make people 3 times more susceptible.

Eva Vega
November 17, 2025 AT 17:58Vancomycin’s ototoxicity profile is still grossly underappreciated in clinical workflows. Even with therapeutic drug monitoring (TDM) optimized for nephrotoxicity, we’re missing the pharmacokinetic-pharmacodynamic (PK-PD) nuance that drives cochlear accumulation. Peak concentrations >80 mcg/mL-regardless of troughs-are the real culprit. The inner ear lacks efflux transporters, so drug sequestration is inevitable with repeated dosing. We need mandatory baseline and serial audiometry for patients on >7-day courses, especially with concomitant loop diuretics. It’s not resource-intensive; it’s negligence to skip it.
Matt Wells
November 19, 2025 AT 06:07It is, indeed, a matter of considerable concern that vancomycin continues to be administered without rigorous adherence to evidence-based dosing paradigms. The persistence of the 15–20 mcg/mL trough target, despite robust meta-analytic data demonstrating no additional bactericidal efficacy beyond 10 mcg/mL, reflects a troubling inertia within institutional protocols. Moreover, the concomitant use of piperacillin-tazobactam-despite a documented 131% increased risk of acute kidney injury-remains de facto standard of care in many ICUs. This is not clinical practice; it is institutionalized complacency.
George Gaitara
November 19, 2025 AT 13:10Let’s be real-vancomycin is a relic. We’re still using a 1950s drug because Big Pharma doesn’t want to fund new antibiotics that won’t make them billions. The fact that we’re still debating whether to check hearing on patients who’ve been on it for 10 days is absurd. Meanwhile, we’re paying $50K/year for cochlear implants while ignoring that we could’ve prevented it with a $200 audiogram. And don’t get me started on how hospitals won’t pay for AUC monitoring because ‘it’s too expensive’-until the lawsuit comes in. Then suddenly, it’s ‘we should’ve done this.’ Classic.
Deepali Singh
November 20, 2025 AT 05:22It’s not just about troughs or peaks. The real issue is heterogeneity in drug metabolism. MT-RNR1 mutations predispose to ototoxicity regardless of renal function, yet we don’t screen. We don’t even test. We just assume ‘normal creatinine = safe.’ That’s not medicine. That’s statistical gambling. And the fact that only 37% of hospitals have audiometry protocols? That’s not a gap-it’s a systemic failure masked as protocol.
Sylvia Clarke
November 21, 2025 AT 11:53Vancomycin isn’t evil-it’s just misunderstood. Like a chainsaw in the hands of someone who’s never read the manual. 🛠️ We’ve got the tools: AUC monitoring, baseline audiograms, risk stratification scores, even AI-driven dosing platforms. But we’re still clinging to 1990s habits because ‘that’s how we’ve always done it.’ Let’s stop pretending we’re saving lives with vancomycin and start admitting we’re just avoiding the hard work of personalized medicine. If we treated antibiotics like we treat cancer drugs-tailored, monitored, adjusted-we’d save more than just kidneys. We’d save people’s voices, their music, their grandchildren’s laughter.
Jennifer Howard
November 22, 2025 AT 00:10It is absolutely unacceptable that any physician would administer vancomycin without obtaining a comprehensive baseline audiogram, renal panel, and genetic screening for MT-RNR1 variants. This is not a suggestion-it is a mandatory standard of care. To do otherwise is to knowingly expose a patient to irreversible sensory damage. The fact that this is not universally mandated speaks volumes about the moral decay of modern medical practice. I have personally reported three such cases to the state medical board. If you are not doing this, you are not practicing medicine-you are practicing malpractice.
Abdul Mubeen
November 22, 2025 AT 10:47Let’s not pretend this is about patient safety. The real reason we’re still using vancomycin is because hospital administrators refuse to pay for newer antibiotics. The ‘risk’ of ototoxicity? A distraction. The real agenda is cost-cutting. The CDC, FDA, and big pharma are in cahoots-vancomycin is cheap, easy to stock, and generates no liability for them. But when a patient goes deaf? That’s when the lawyers come. And suddenly, everyone’s talking about ‘evidence-based practice.’ Coincidence? I think not.
mike tallent
November 23, 2025 AT 05:20Y’all are overcomplicating this. 🤓 Low dose (15-20mg/kg/day), max 4g, check creatinine every 48h, avoid piperacillin combo unless no choice, and if they’re over 65 or on furosemide? Get the audiogram. Done. AUC monitoring? Sweet if you’ve got it, but not everyone’s in a fancy hospital. This isn’t rocket science-it’s basic vigilance. And yeah, if your patient starts saying ‘huh?’ when you talk, STOP THE DRUG. No waiting for labs. 🚨
Joyce Genon
November 24, 2025 AT 03:14Everyone’s acting like vancomycin is the only problem here, but let’s be honest-this entire conversation is a symptom of a broken system. We’re not talking about vancomycin toxicity; we’re talking about how medicine has become a bureaucratic performance art where guidelines are written by committees who’ve never seen a real patient, and then enforced by residents who are sleep-deprived and drowning in EHR alerts. We have 17 different protocols for vancomycin dosing, 12 different risk scoring systems, and yet the most common cause of nephrotoxicity is still the same: someone forgot to check the creatinine because they were too busy documenting a ‘patient preference’ for oat milk in their coffee. The real toxicity isn’t in the drug-it’s in the culture.
John Wayne
November 25, 2025 AT 17:13It’s amusing how quickly the medical community pivots to ‘precision medicine’ when it’s convenient. Vancomycin has been used for 70 years. We didn’t need AUC monitoring or genetic screening to save lives before. Now, because some papers show a 9% reduction in AKI, we’re suddenly treating it like a biologic. The truth? Most patients don’t need vancomycin at all. The real solution isn’t better monitoring-it’s better diagnostics. Stop treating every fever as MRSA. Stop defaulting to vancomycin because you’re afraid of missing something. That’s not medicine. That’s fear-driven prescribing.