Warfarin-NSAID Bleeding Risk Calculator
This tool estimates your bleeding risk when combining warfarin and NSAIDs based on key clinical factors. Results are for informational purposes only and do not replace medical advice.
Your Bleeding Risk Assessment
Emergency Warning: If you experience any of these symptoms, stop NSAID immediately and seek emergency care:
- Black/tarry stools or vomiting blood
- Uncontrollable nosebleeds or bleeding gums
- Sudden severe headache, confusion, or dizziness
- Unexplained bruising or weakness
Why mixing warfarin and NSAIDs can be dangerous
If you're taking warfarin to prevent blood clots, adding a common painkiller like ibuprofen or naproxen might seem harmless. After all, millions of people use these drugs for headaches, back pain, or arthritis. But when warfarin and NSAIDs are taken together, the risk of serious bleeding goes up dramatically - sometimes by more than four times. This isn’t just a theoretical concern. It’s a real, documented danger that sends people to the hospital every year.
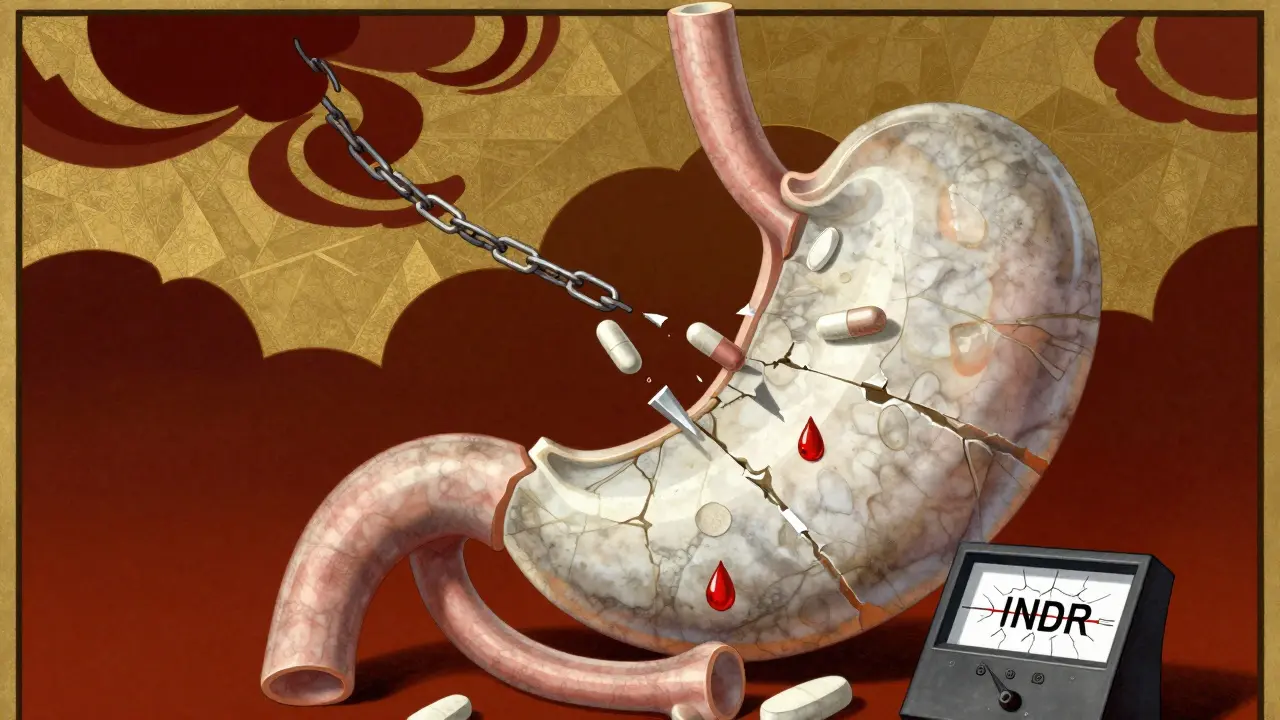
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without enough of these factors, your blood takes longer to clot. That’s the goal - to stop dangerous clots from forming in your heart or legs. But when you add an NSAID - a class of drugs that includes ibuprofen, naproxen, diclofenac, and even aspirin - you’re adding another layer of risk. NSAIDs don’t just relieve pain. They also mess with your platelets, the tiny blood cells that help seal cuts and bruises. They do this by blocking an enzyme called COX-1, which reduces thromboxane A2, a chemical that tells platelets to stick together. So now you’ve got two systems working against clotting: warfarin slowing down the production of clotting proteins, and NSAIDs making platelets less responsive.
This isn’t a simple add-on effect. It’s a synergy. The combination creates a perfect storm. Your blood doesn’t just clot slower - it becomes harder for your body to stop bleeding once it starts. And the most common place this goes wrong? Your gut.
The gut is ground zero for bleeding
NSAIDs damage the stomach lining by reducing protective prostaglandins. That’s why long-term use can cause ulcers. When you add warfarin to the mix, that damaged lining becomes a ticking time bomb. A 2024 meta-analysis found that people taking both drugs had twice the risk of gastrointestinal bleeding compared to those on warfarin alone. That means black, tarry stools, vomiting blood, or sudden dizziness from blood loss - all signs you need emergency care.
But it’s not just the stomach. Brain bleeds, lung bleeds, and urinary tract bleeds also rise. One major study showed that the risk of intracranial hemorrhage jumped 3.2 times when NSAIDs were added to warfarin. Even minor injuries - a bump on the head, a fall, a nosebleed - can turn serious. And because warfarin’s effects build up over days, you might not notice anything wrong until it’s too late.
Not all NSAIDs are the same
Some NSAIDs are riskier than others. Naproxen carries the highest bleeding risk - nearly four times higher than warfarin alone. Diclofenac isn’t far behind, tripling the risk. Ibuprofen is a bit safer, but still increases bleeding by nearly 80%. Meloxicam, often thought of as a gentler option, was flagged in one study as an independent predictor of dangerous INR spikes. That means even if you’re on a low dose, meloxicam can push your INR up enough to require emergency intervention.
And here’s something most people don’t realize: it’s not just about the dose. Even low-dose aspirin, often taken for heart protection, can interfere with warfarin. It doesn’t matter if you’re taking 81 mg or 325 mg - it still affects platelets. And if you’re taking both, you’re doubling down on risk without doubling down on benefit.
Who’s most at risk?
Some people are more vulnerable than others. If you’re on more than 40 mg of warfarin per week, your body is already struggling to maintain balance. Add an NSAID, and your INR can spike by 15% or more - enough to trigger bleeding. Older adults, especially those over 70, are at higher risk. So are people taking other medications that interact with warfarin, like antibiotics or antifungals. Even something as simple as changing your diet - eating more leafy greens one week, less the next - can throw your INR off. Adding an NSAID on top of that? It’s a recipe for disaster.
Another red flag: low baseline INR. If your INR is usually on the lower end of the target range (say, 2.0), you have less room for error. A small rise from an NSAID can push you into dangerous territory fast. That’s why doctors often avoid NSAIDs entirely in these patients.
What to do instead
You don’t have to suffer in pain. There are safer alternatives. Acetaminophen (paracetamol) is the go-to for most people on warfarin. Up to 3,000 mg a day is generally safe, as long as you don’t have liver disease. Topical creams with menthol or capsaicin can help with joint pain. Heat packs, physical therapy, and even acupuncture can reduce reliance on pills.
If you absolutely need an NSAID - say, after surgery or for severe arthritis - your doctor might prescribe a proton pump inhibitor (PPI) like pantoprazole to protect your stomach. But even then, you’ll need more frequent INR checks. The standard advice is to test your INR within 3 to 5 days after starting the NSAID, then weekly while you’re on both drugs. Don’t assume your last test is still valid.
What the guidelines say
The American College of Chest Physicians and the European Society of Cardiology both warn against combining NSAIDs with warfarin unless there’s no other option. Even then, they recommend the lowest possible dose for the shortest time. Harvard Health and the FDA both include strong warnings in their labeling: “Concomitant use may increase the risk of bleeding.”
And yet, studies show that nearly 3 out of 10 people on warfarin still get prescribed an NSAID. That’s not just a gap in care - it’s a preventable crisis. Many doctors assume patients are taking over-the-counter painkillers and don’t ask. Many patients don’t think to mention them. That’s why it’s on you to speak up.
What to watch for
If you’re on both drugs, know the warning signs of bleeding:
- Unusual bruising, especially without injury
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Dark, tarry stools or blood in stool
- Red or pink urine
- Sudden severe headache, dizziness, confusion (possible brain bleed)
- Unexplained weakness or fatigue (sign of anemia from blood loss)
If any of these happen, stop the NSAID immediately and call your doctor. Don’t wait. Bleeding from this interaction can be fatal.
Bottom line
Warfarin and NSAIDs don’t play well together. The science is clear, the risks are high, and the consequences can be deadly. Avoiding this combination is the safest move. If pain is keeping you from living your life, talk to your doctor about alternatives. Don’t risk your health for a quick fix. Your body already has enough to manage - don’t make it harder.

Becky M.
February 3, 2026 AT 08:48Just had my grandma on warfarin for 8 years and she never took anything stronger than tylenol. I don't get why people think OTC means harmless. It's not like ibuprofen is a vitamin.